Auditing the identification and inpatient management of acute malnutrition in infants under six months in Malawi
Summary of MSc thesis
By Laura White
Laura White is a Canadian-trained registered dietitian who recently completed an MSc in Nutrition for Global Health at the London School of Hygiene and Tropical Medicine. She is currently working in Papua New Guinea as a clinical nutrition advisor under the Nutrition and Dietetics Support Programme implemented by the National Department of Health and Voluntary Service Overseas.
Laura would like to thank her MSc supervisor, Dr. Marko Kerac, along with Dr. Laura Newberry at Queen Elizabeth Central Hospital (QECH), Malawi for their support in completing this project. Many thanks also to the staff of the paediatric nursery ward of QECH, who collected all the data for this audit through their daily work, and to her hard-working data entry assistant, A.T.
Location: Malawi
What we know: Severe acute malnutrition (SAM) in infants<6m is a significant global health burden. WHO 2013 guidance recommends community-based management for uncomplicated cases; in practice, management remains inpatient-based.
What this article adds: An audit (quantitative and qualitative data) was conducted of inpatient management of infants<6m admitted to the Queen Elizabeth Hospital in Malawi over a 23-month period. Substantial missing/compromised data were found: 15.9% had no admission weight, while 92% of weights and 81% of lengths were rounded figures. The prevalence of SAM and moderate acute malnutrition (MAM) were 12.1% and 9.9% respectively. SAM infants had 9.28 times higher odds of mortality (p<0.001) than healthy-weight counterparts. Among malnourished infants, there was no significant difference in weight gain during admission, proportion of infants reaching normal nutrition status on discharge or mortality with the recruitment of an infant feeding specialist nurse (IFSN) or with baby-friendly hospital initiative (BFHI) training, during the audit period. The utilisation of supplementary suckling dropped over time. Use of infant formula increased (this related to supplies timing rather than interventions). Overall implementation of national SAM guidelines for infants<6m remained low, despite IFSN and BFHI; challenges included low staff knowledge of, and confidence in, guideline implementation. To address highlighted gaps, staff education and training, more research on anthropometric criteria for screening infants< 6m and a randomised controlled trial (RCT) on the impact of specialist feeding support are needed.
Background
Severe acute malnutrition (SAM) in infants less than six months (infants<6m) is a significant global health burden. Persisting misperceptions that infants cannot be malnourished, coupled with low staff confidence in identifying and managing malnutrition in this age group, means valuable opportunities to identify and treat nutrition problems are being missed (Kerac et al, 2012). As malnutrition in infancy has immediate and long-lasting effects, it is vital to improve the evidence base regarding the management of malnutrition in infants<6m.
In Malawi, it is estimated that 4.1% of infants<6m are severely wasted, compared with 2.6% of children aged 6-59 months (National Statistical Office, 2010). Infants<6m have been included in Malawi’s malnutrition guidelines since 2006; treatment is solely inpatient-based and centres around supplementary suckling for infants who can be breastfed (Malawi Ministry of Health, 2012). This technique uses a nasogastric tube attached to the nipple to deliver supplementary milk while the infant suckles at the breast. Stimulation of the nipple increases maternal breast milk supply and, as the process progresses, less supplementary milk is given via the tube as the infant receives more milk from the breast. Despite these long-standing national guidelines, limited resources – particularly of staff – have meant that they are rarely implemented due to the ample maternal counselling and support required to achieve success (Lelijveld et al, 2013).
In August 2013, funding was obtained to hire an infant feeding support nurse (IFSN) at Queen Elizabeth Central Hospital (QECH), Malawi’s biggest public hospital, to implement the existing Malawi severe acute malnutrition (SAM) guidelines for infants<6m. Following her appointment, coincidentally baby-friendly hospital initiative (BFHI) training of all paediatric nursery ward (PNW) staff occurred one year later. Components of the BFHI, such as training staff in necessary skills to support mothers to establish or manage breastfeeding, are complementary to national SAM guidelines and therefore have the potential to reinforce the IFSN’s efforts.
Audit outline
The aim of this audit was to review the impact of implementing existing Malawi SAM guidelines on the PNW at QECH as first implemented by the IFSN alone, and later supported by a wider group of BFHI-trained staff. The specific objectives of the audit were to:
- Examine the management of malnourished infants by comparing treatment and discharge information to the national SAM guidelines for the different periods of implementation, specifically:
- the burden of malnutrition on the PNW (prevalence and links with mortality);
- the proportion of infants exclusively breastfed (EBF) at discharge;
- weight gain over the course of admission; and
- the proportion of infants reaching normal nutritional status at discharge
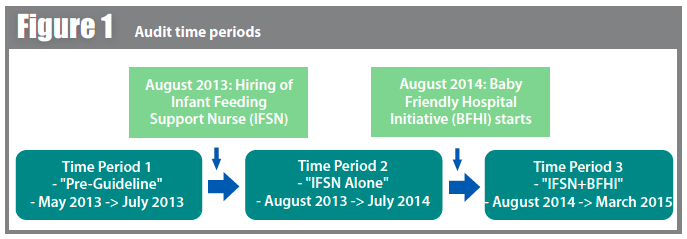
The audit involved retrospective, quantitative (infant data) analysis supplemented with qualitative (staff perceptions) data to evaluate the impact of implementing SAM guidelines and BFHI on the ward, but was primarily descriptive in nature. The three time periods for data collection and analysis of the audit are detailed in Figure 1.
 Findings
Findings
Identifciation of malnourished infants
For this component of the audit, admission data recorded in the ward register was analysed to determine the burden of acute malnutrition on infants<6m admitted to the PNW at QECH. Results demonstrated that the collection of routine clinical data is currently a barrier to the identification of malnutrition on the PNW. Substantial missing data (15.9% of admissions had no weight) and heavy rounding of anthropometric measures (92% of weights and 81% of lengths) were discovered by the audit. Data from the ward register was analysed for all patients admitted during the time period and showed that 56.1% of the admissions were male; the median age at admission was eight weeks old; 23.4% of infants were HIV-exposed; and 86.5% of all admissions were exclusively breastfed on admission. As HIV status was recorded using two different sets of indicators (exposure and reactivity status), data were simplified to recording if an infant was exposed for analysis purposes (assumed all reactive infants were exposed).
Of the 3,651 infants admitted to the ward from May 9 2013 until March 31 2015, 2,405 (65.9%) infants had sufficient admission data recorded to be included in the prevalence of malnutrition calculations, using ENA for SMART software to calculate weight-for-length Z scores (WLZ). The overall prevalence of SAM (WLZ<-3) and MAM (-3<WLZ<-2) respectively were 12.1% and 9.9%. Comparing WLZ calculated by ENA for SMART software to the WLZ information recorded in the ward register reveals that 30% fewer cases of SAM and 41.2% fewer cases of MAM were identified by staff in the ward register than could be calculated using ENA.
SAM infants had 9.28 times higher odds of mortality (p<0.001) than their healthy-weight counterparts. The missed opportunities to identify SAM and MAM is therefore an important finding, as acutely malnourished infants have a higher risk of death on admission and interventions are available. Early detection of SAM infants and proper treatment following the Malawi SAM guidelines are likely to improve mortality outcomes of these vulnerable infants.
Management of acutely malnourished infants
Additional data were collected on malnourished infants (n=179) admitted to the ward focusing on the management of SAM treatment for these infants during admission. Across the whole audit, implementation of national SAM guidelines for infants<6m remained low, although some variation was seen across the time periods. While the mean average weight gain (g/day) decreased from 60g/day pre-guideline (95% CI: -36, 158), to 15g/day with both the IFSN and BFHI (95% CI: 4, 27), the changes were non-significant (p=0.353). Pre-guideline, 22.2% of infants reached normal nutrition status at discharge, as opposed to 16.7% of those with IFSN+BFHI, although the small sample size used for these calculations impacts significance of these results (p=0.806). Mortality among SAM infants stayed constant across the three time periods (p=0.125), with an overall mortality rate of 17.9%.
To summarise, among malnourished infants, no significant difference in weight gain during admission, proportion of infants reaching normal nutrition status upon discharge or mortality was observed with the start of IFSN or BFHI. Although not collected formally, it was observed that the IFSN schedules regular check-up appointments when infants are discharged to track weight gain and any relapse, which is part of the national SAM guidelines for follow-up (the proportion of infants who return for these appointments is unknown as it is not collected as part of the audit).
The utilisation of supplementary suckling dropped over time (17.4% pre-guideline to 2.4% with IFSN+BFHI), p=0.006. This could possibly be attributed to the IFSN accurately identifying which infants needed this treatment, compared with the pre-guideline period when it was used with almost one-fifth of infants (despite a large number of infants during this time being misdiagnosed with SAM). The biggest difference observed was the number of infants discharged on infant formula (p<0.001), reaching as high as 52.7% with the start of the IFSN. However, in staff discussions it was discovered this related to the supply of infant formula on the ward (shortages in supply occurred during pre-guideline and in IFSN+BFHI time periods) and cannot be causally linked with the staff interventions occurring at that time. It should be noted that at QECH nursery, infant formula is preferentially prescribed over F75 therapeutic milk for malnourished infants where EBF is not possible (orphans, cleft lip/palate, congenital heart disease, etc). The formula is not provided by the hospital, which is why supplies vary over time. On admission, it was determined that 71.5% of malnourished infants were exclusively breastfed with no significant differences in proportion of infants EBF across the time periods (p=0.484). On discharge, across the three time periods, 59.2% of infants were EBF with no significant differences seen in the proportion of infants EBF over the time periods (p=0.295). It should be noted that although non-significant changes were seen over time, 65.2% of infants were EBF on admission pre-guideline, and 60.9% at discharge. For the IFSN+BFHI period, 66.7% were EBF on admission and 69.0% EBF at discharge.
Conclusions
Although no significant difference in progress and outcomes of infants<6m with the start of IFSN or IFSN+BFHI was found, the small sample size for each time period (n=23 pre-guideline, n=114 with IFSN, n=42 with IFSN+BFHI) and the use of operational data which varied in quality, limit interpretation of the audit findings and the ability to draw definitive conclusions on the impact of an IFSN. Contextual information collected through staff focus group sessions highlighted the challenges that exist in implementing national SAM guidelines, including supplies, staff knowledge of the guidelines, and confidence in implementing the guidelines. These focus group sessions also revealed that over the previous few months, the IFSN had been the only staff member calculating the WLZ for all admissions to the ward (identifying malnourished infants) and is the only staff member providing formal breastfeeding education. A future RCT that explores whether a dedicated IFSN improves outcomes is needed to provide a definitive answer.
Overall, this audit highlights the importance of addressing current gaps regarding identification and management of malnutrition for infants<6m. Staff education on the importance of robust, routine anthropometric measurements and the calculation of WLZ scores on admission to identify malnourished infants is the first priority to address these gaps and prevent deaths attributable to malnutrition in the short term. Secondly, contextual information suggests that training sessions on infant malnutrition and infant feeding would help staff feel more confident in dealing with malnourished infants. Longer term, more research is needed to expand the detection methods available for MAM/SAM screening in infants<6m (for example, MUAC or weight-for-age) and further explore the barriers regarding implementation of the Malawi SAM guidelines. Lastly, future RCTs are needed to examine more clearly the impact of an IFSN and the effectiveness of implementing SAM Guidelines on infant outcomes.
For more information, contact: Laura White
References
Kerac M, Tehran I, Lelijveld N, Onyekpe I, Berkley J, Manary M, 2012. Inpatient treatment of severe acute malnutrition in infants aged <6 months. WHO.
Lelijveld N, Mahebere-Chirambo C, Kerac M, 2013. Carer and staff perspectives on supplementary suckling for treating infant malnutrition: Qualitative findings from Malawi. Maternal and Child Nutrition 2013; pp593-603.
Ministry of Health, 2012. Malawi Severe Acute Malnutrition Guidelines.
National Statistical Office, 2010. Malawi Demographic and Health Survey 2010.