Partnership and accountability in the South Sudan Nutrition Cluster (2015-2017)
By Isaack Biseko Manyama
Isaack Manyama is the Nutrition Cluster Coordinator for South Sudan. He has 24 years’ experience in the nutrition sector. Previous roles have included Team Leader of the Emergency Coordination Unit (ENCU) in the Early Warning and Response Directorate of the Ministry of Agriculture in Ethiopia, Primary Health Care Officer for UNICEF Tanzania and Senior Nutritionist at the Tanzania Food and Nutrition Centre.
The findings, interpretations and conclusions in this article are those of the authors. They do not necessarily represent the views of UNICEF, its executive directors, or the countries that they represent and should not be attributed to them.
Location: South Sudan
What we know: Acute malnutrition remains a major public health emergency in several parts of South Sudan, driven by ongoing conflict and displacement, poor access to health services, inadequate water, sanitation and hygiene, and chronic food insecurity.
What this article adds: The Nutrition Cluster is well established in South Sudan and involves a Strategic Advisory Group, thematic technical working groups, including on quality and accountability to the affected population, and a rapid response mechanism task force. Partnership and accountability is a cross-cutting theme in assessment, response gap analysis, response planning, costing, implementation and monitoring. Experiences reflect the key role the Nutrition Cluster plays in brokering partnerships, resolving differences and holding responders to account. Transparency across all aspects of the humanitarian project cycle, together with trust and open dialogue among all stakeholders, is critical. High staff turnover and competition for operational opportunities stifle good partnership and accountability. Sustained capacity building, monitoring, awareness raising and lesson learning are key.
Background
Nutrition context
Acute malnutrition remains a major public health emergency in several parts of South Sudan. Over 1.1 million children are estimated to be acutely malnourished in 2017, of which 706,427 (63.7%) are expected to be reached with curative nutrition services (75% of those children with severe acute malnutrition (SAM) and 60% of children with moderate acute malnutrition (MAM)). The May 2017 integrated phase classification (IPC) estimated that 6.1 million people (50 per cent of the population) would be severely food insecure in June/July 2017, compared to 5.5 million (45 per cent) people in May 2017. This is the greatest number of people ever to experience severe food insecurity (IPC phases 3, 4 and 5) in South Sudan.
As expected, the 2017 food security situation, which builds on food insecurity and deterioration of livelihood assets from previous years, has been manifesting in increased levels of acute malnutrition. The proportion of SMART surveys reporting critical levels of global acute malnutrition (GAM ≥ 15 per cent) increased from 77 per cent (of 40 surveys conducted from January to September 2016) to 82 per cent (of 33 surveys conducted in the same period in 2017). A peak of 36.1 per cent GAM was found in Twich County, classifying it as ‘extremely critical’. Admissions in selective feeding programmes increased from January to July 2017, with an overall combined 19 per cent increase in both SAM and MAM compared to the same period in 2016. Key drivers of the high levels of acute malnutrition across South Sudan include: ongoing conflict and displacements; poor access to basic services; economic crisis, with increased staple food prices associated with the devaluation of the South Sudanese Pound; disease outbreaks; inadequate dietary intake in terms of both quality and quantity; low coverage of sanitation facilities; and poor hygiene practices.
Nutrition Cluster partners and other stakeholders continuously support the Ministry of Health (MoH) in responding to the ongoing nutrition emergency. While the nutrition situation remains highly insecure, famine is no longer occurring in Leer and Mayendit Counties, and further deterioration was prevented in Koch and Panyijiar Counties of former Southern Unity State due to immediate and sustained multi-sector humanitarian assistance delivered to the affected population from March to May 2017. The MoH with UNICEF, the World Food Programme (WFP), the World Health Organization (WHO) and Save the Children International (SCI) have continued to lead Nutrition Cluster partners in developing and finalising three important national guidelines, including their respective implementation tools and training packages: community-based management of acute malnutrition (CMAM); maternal, infant and young child nutrition (MIYCN); and inpatient management of SAM.
The South Sudan Nutrition Cluster
The Nutrition Cluster in South Sudan was established in 2010 and currently comprises 64 active partners, including 43 national and international non-governmental organisations (NGOs) implementing nutrition responses on the ground. The cluster is coordinated through a fortnightly meeting, chaired by the Nutrition Cluster Coordinator (NCC). Several regular bilateral and tripartite meetings are also held with partners and other stakeholders, including donors, to provide updates and address or respond on assessments, monitoring and funding issues. In addition, meetings between the Nutrition Cluster coordination team -and donors are held once every two months with an agenda which is agreed with the donors. The strategic direction of the Nutrition Cluster is decided by the Strategic Advisory Group (SAG), composed of MoH, United Nations (UN) agencies, national and international NGOs as well as representation from the Health Pool Fund (HPF), a donor that applied to be a member of the reformed SAG (August 2017).
Several thematic working groups (TWGs) have been formed to coordinate specific technical areas on behalf of Nutrition Cluster partners. These include: CMAM TWG, which is responsible for CMAM technical issues, scale-up and revision/development of CMAM guidelines, support in the review of the stabilisation centre guidelines, and CMAM training rollout to the states; and the Nutrition Information Working Group (NIWG), responsible for coordinating emergency nutrition data collection (based on SMART/Rapid SMART surveys), and analysis, validation and dissemination to the cluster members through the fortnightly cluster meetings and other cluster-approved channels. The NIWG also represents the Nutrition Cluster in IPC preparation/revision and other inter-cluster information-related activities. The MIYCN TWG, which was established in 2015, is responsible for all MIYCN issues, including supporting the MoH in the development of national MIYCN guidelines, strategy documents and training packages.
The Rapid Response Mechanisms (RRM) Task Force was also established in 2015 to coordinate outreach services through the RRM, implemented by UNICEF and WFP, as well as short-term response approaches implemented by Medair and Action Against Hunger (AAH). Lastly, the Quality and Accountability to Affected Population (QAAP) TWG is responsible for ensuring improved assessment of quality services and integration of the Nutrition Cluster Accountability to Affected Populations (AAP) framework into partners’ projects.

Needs assessment and analysis
Needs assessment
Nutrition Cluster needs assessments are conducted through a number of assessment and information-gathering methodologies. First, periodic SMART surveys are conducted during the pre-harvest period (March-September) and the post-harvest period (October-February) in priority counties. Ad hoc surveys are also conducted based on IPC analysis or where there is a need to confirm or clarify the status of a reported deteriorating nutrition situation based on mid upper arm circumference screening. By the end of September, a total of 33 SMART surveys had been conducted, of which 27 reported critical levels of acute malnutrition (GAM ≥ 15 per cent).
Food Security and Nutrition Monitoring Systems (FSNMS) are conducted twice per year, in June/July and November/December. These surveys highlight the nutrition situation at state level. Recently, the FSNMS team agreed to increase the sample sizes to integrate at least four SMART surveys at county level with the FSNMS surveys. The June/July 2017 survey also indicates deterioration of the nutrition situation, with consistently higher levels of GAM than those reported in 2016 in the same period. Specifically, eight out of the nine states assessed reported GAM levels above the 15 per cent emergency threshold, compared to seven out of ten states during the same period in 2016.
IPC classification is one of the methods that provide guidance on the specific county-level and overall food security and nutrition situation in the country and identifies areas with information gaps. As mentioned above, such areas are prioritised for ad hoc SMART surveys, especially when food security indicators signal deterioration. Based on the available IPC analysis, the food security and nutrition situation deteriorated consistently in the last three years (2015-17).
Good quality monthly new admissions programme data (therapeutic feeding programme (TFP) and targeted supplementary feeding programme (TSFP)) is very useful in tracking how the nutrition situation is evolving at site, county, state and national levels. It increases understanding of whether the observed situation is usual or unusual. For the last three years (2015-2017), monthly admissions trends have informed the Nutrition Cluster partners and stakeholders on whether the situation is stable or improving or a crisis is imminent and whether timely actions are needed. The data guides the need for supply/procurement top-up and delivery to areas of need and deployment of surge staff to balance quality and workload, among other necessary activities.
Response gap analysis
At the beginning of 2016, the Nutrition Cluster initiated nutrition response gap analysis, focusing on outpatient therapeutic programme (OTP)/TSFP geographic coverage in health facilities, expected optimal coverage (distance from one site to another) and population size. This approach and tool was criticised by partners as the process of identifying gaps was subjective. In view of this, the Nutrition Cluster, through the QAAP TWG, coordinated revision of the tool in 2017. The response gap analysis tool was revised and expanded to include assessment of gaps in service quality based on several weighted indicators; structural status of nutrition sites; and geographic coverage of nutrition sites, with clear scoring and decision-making rules for characterising a site as under-performing. The tool was presented and reviewed by partners and approved. It was piloted at the end of August 2017 and was due be rolled out in December 2017 at the time of writing.
Gaps in response are also identified by cluster field monitoring visits jointly carried out with UNICEF, WFP or the MoH. Identified gaps are discussed with the partners concerned and an action plan is drawn up to address them, with regular updates provided to the cluster coordination team.
Cluster targets in all programme areas
The Nutrition Cluster targets for both SAM and MAM are estimated based on the existing burden coupled with actual and planned partners’ capacity to expand, as well as previous year performance coverage and absolute number of children enrolled in OTP and TSFP. For example, if 90-100 per cent of the target was attained and the situation is expected to be similar or worse, subsequent annual targets are set at the same level or increased as necessary. The cluster targets are estimated initially by the cluster coordination team and presented to the SAG members for further guidance before discussion and approval by the all Nutrition Cluster partners.
Challenges related to needs analysis
It is difficult to link emergency and long-term development information systems, partly because development nutrition information is scant and not readily available, with a lack of national survey data for comparison of levels of acute malnutrition. Insecurity limits coordination and assessments in conflict-affected states. It is also difficult to conduct assessments in all counties due to limited capacity and the prohibitive cost of SMART surveys (US$20,000 to US$30,000 depending on the location, security and logistics needed and whether implemented by a consultant). There is limited funding to sustain the number of annual surveys conducted over the coming years. The quality of some nutrition survey results is sub-optimal. In such situations, the NIWG may reject the SMART survey; one survey was rejected in May/June 2017 due to poor quality of results. There is high staff turnover among partners and therefore there is a need for regular training on SMART surveys. The latest training was done in June 2017.
To try and overcome these challenges, state-level results are extrapolated to county level, where the information gap is plausible and accepted by stakeholders. However, in some situations this can overestimate the levels of acute malnutrition in low-prevalence counties. NIWG collective review and discussion of survey results fosters transparency and credibility and instils a sense of responsibility and accountability among both partner and NIWG members. Follow-up, capacity building and feedback to partners improve information/data quality (accuracy, timeliness, comprehensiveness/reporting rate and records). Improved information management is a continuous process requiring time, dedicated staff and sufficient funding.
Response planning
For the last four years (2014-2017), Nutrition Cluster response planning has focused on the following three priorities: providing life-saving services on management of acute malnutrition (TFP/TSFP); increased access to prevention programmes (blanket supplementary feeding programme (BSFP) and targeting pregnant and lactating women (PLW) and maternal infant and young child nutrition (MIYCN); and enhanced nutrition situation analysis, monitoring and coordination. A fourth priority – integration of nutrition responses with other nutrition-sensitive interventions from other sectors (including health, water, sanitation and hygiene (WASH) and food security and livelihoods (FSL)) – was introduced in 2017.
Response planning process
First, the timelines for development of the national and cluster Humanitarian Response Plan (HRP) is drafted by the United Nations Office for the Coordination of Humanitarian Affairs (OCHA), discussed in the Inter-Cluster Working Group (ICWG) and approved by the Humanitarian Country Team (HCT). Once approved, the Nutrition Cluster coordination team drafts the cluster response plan based on available assessment and response information from different sources (SMART, programme data, FSNMS, IPC, the Humanitarian Needs Overview (HNO) and priority response needs. The response (actions) are presented to SAG members for review before being presented to Nutrition Cluster partners for further discussion, review and approval. The cluster response plan is then submitted to OCHA for ICWG-level peer review/defence and comments. Based on the comments/inputs from OCHA/ICWG, the response plan is finalised and submitted to OCHA.
Contribution and participation of partners and government is critical. During the SAG/partners discussion phase, the cluster coordination team must engage respective government ministries to ensure buy-in and support. For example, ad hoc meetings were organised by the cluster coordination team, during which partners reviewed the 2015, 2016 and 2017 drafts and enriched it accordingly before it was submitted to OCHA for defence. While there was limited involvement of government in the initial stages of the 2015 plan, government reviewed the final cluster caseloads/targets and situation analysis in the 2017 response plan.
Costing
The total funding requirements published by OCHA, coordinated by the Nutrition Cluster, reflects frontline and pipeline needs. Nutrition Cluster coordination costs are not part of the HRP budget; these are covered by UNICEF. The cost for HRP was determined using two different approaches in 2016 and 2017. The first approach, used in 2016, was based on OCHA’s guidance. The cluster’s funding requirement was determined based on how much funds the cluster could raise in 2015 (including carry over from 2014). A 10 per cent contingency of the total cluster-secured funding for 2015 was added to determine the funding requirement for 2016. This approach was used for all clusters. Partners recommended estimating the funding requirements based on need, but the approach for 2016 had already been decided by OCHA/HCT. The total budget (funding requirements) was communicated to all cluster partners. In 2017, clusters were allowed to estimate funding requirements based on need. With respect to the Nutrition Cluster, the funding requirement was determined by multiplying the number of beneficiaries with the estimated costs of managing one case of PLW and children enrolled in TFPs, TSFPs and BSFPs. The sum of these individual costs was taken as the total requirement for the programming identified by the Nutrition Cluster in 2017. In practice, the total HRP budget does not mean that all the nutrition requirements are reflected/covered – a funding ceiling is applied by OCHA for all clusters, beyond which clusters cannot increase funding even if needed. Notwithstanding, mid-reviews provide an opportunity for clusters to review their respective humanitarian needs, targets and funding requirements. In situations where there is an unforeseen major crisis/emergency, as in the case of the Declaration of famine in February 2017, the Nutrition Cluster may revise its funding requirements for counties affected and additional funding may be provided by donors to meet heightened needs.
Since different costing approaches were used, it is difficult to compare funding requirements across the years. The 2016 costing/budget was not based on need and was instead very much driven by donor’s willingness to fund; 2016 cluster budgets had to be cut considerably to fit within the budget ceiling. Determining funding requirements based on funding status misleads donors/stakeholders that the project requires less resources, while the unmet funding needs in reality are huge. It is difficult to separate projects that are emergency per se and those that focus on development. As a result, partners continue to advocate for projects whose resources are not reflected in the HRP/online project system (OPS). Donors can still fund projects outside of the HRP/OPS, which arguably undermines the importance of the HRP (among the donors and partners themselves). A separate funding tracking system (FTS) is needed to capture projects outside the HRP-FTS in the OPS in future.
Response implementation
Several emergency nutrition response modalities are coordinated by the Nutrition Cluster in South Sudan. These include: static/mobile, RRM, inter-cluster response mission (ICRM), emergency response team (ERT)/multi-sector emergency team (MET) and survival kit (see Box 1). In terms of supplies, partners agreed in 2013/2014 that UNICEF and WFP would be responsible for procurement and delivery of the core pipeline (ready-to-use therapeutic food (RUTF) and ready-to-use supplementary food (RUSF)) and other supplies to project implementation counties/sites. While WFP delivers the supplies to partners using its own logistics unit assets, UNICEF relies on private transporters and the Logistics Cluster in transporting SAM supplies from designated state-level warehouses to partners’ operational counties/sites. Few partners procure their own buffer stock to be used in case of constraints in the core pipeline status. Médecins Sans Frontières (MSF) procures its own supplies most of the time and occasionally accesses the core pipeline supplies.
Box 1: Emergency nutrition response modalities
Static/mobile
Once an area is designated an emergency (most), UNICEF and WFP sign programme cooperation agreements (PCAs) and field-level agreements (FLAs) for management of SAM and MAM respectively in static settings or mobile settings, depending on what the situation on the ground will allow. The package includes funding for staff, rehabilitation of nutrition sites, monitoring and supervision, access to core pipeline supplies and reporting tools. These agreements are reviewed at any time of the year (UNICEF) and in the last quarter of the year (WFP), with a provision for amendments/addendums to the existing agreement in the course of the year should there be increased caseloads.
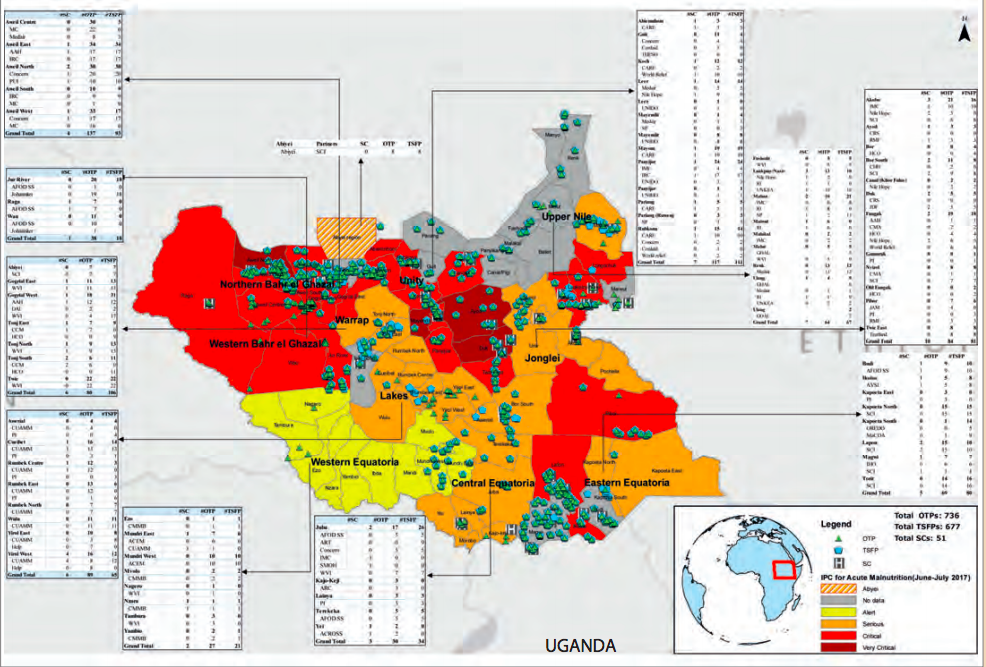
By the end of June 2017, a total of 43 partners (international and national NGOs)) had active PCAs (with UNICEF) and FLAs (with WFP), covering a total of 704 OTP and 707 TSFP sites in 69 out of 79 counties across the country (see Figure 1). It is important to note that some of the partners are funded bilaterally by donors and also have PCAs/FLAs with UNICEF and WFP; either to secure top-up funding or to secure core pipelines supplies (RUTF and RUSF) centrally procured by the two agencies.
The Nutrition Cluster is also actively involved in identifying response gaps and recommending partners with capacity to implement nutrition response in consultation with both UNICEF and WFP as well as with other donors accordingly.
Rapid response mechanism (RRM)
UNICEF/WFP also directly implement SAM and MAM responses through RRM where there is no partner and needs are high. The RRM remains the preferred modality for reaching women and children in inaccessible areas cut off due to insecurity and/or limited access implemented in collaboration with partners. This modality is usually scaled up when the situation deteriorates. For example, during 2017, a total of 45 RRMs were implemented; 21 in Unity State. This modality was especially used in famine counties where services had been suspended due to insecurity or limited coverage by partners.
Inter-cluster response mechanism (ICRM)
This modality was introduced by the ICWG, coordinated by OCHA, to complement the efforts that were being made by UNICEF/WFP RRMs. The modality of implementation is similar to the UNICEF/WFP RRM; however UNICEF/WFP do not field their own staff, but do provide technical and operational guidance and supplies. Other sectors are involved, including health, WASH, non-food items (NFI) and FSL.
Emergency response team (ERT)/Multi-sector emergency team (MET)
These are short-term response mechanisms coordinated by the Nutrition Cluster and implemented by Medair and AAH. They constitute technical teams of SAM and MAM management (ERT) as well as food security and WASH support (MET). They are deployed for a minimum period of three months to support partners who are overwhelmed by the response or where there are no partners at all. By the end of the three-month period, enough capacity will have been built for any existing partner to take over, or the cluster, in collaboration with UNICEF and WFP, will have identified a partner to respond in those areas.
Survival kit
This is the response mechanism coordinated by OCHA and implemented in areas that are difficult to access, such as displaced populations hiding on an island fearing for their security. The kit is composed of minimum supplies for one household from different clusters, including health, WASH, FSL, NFI and Nutrition. The nutrition component comprises enough BP5 biscuits for two children under five years old per household for five days (there is currently no provision for PLW).
Figure 1: Nutrition situation and presence of nutrition partners in South Sudan, August 2017
MoH, UNICEF, WFP and national and international NGOs engage in capacity building on management of acute malnutrition (CMAM and MIYCN) activities across the country. This is particularly important given the high staff turnover among partners in South Sudan, necessitating the need for continuous training of partners on CMAM and MIYCN annually or sometimes twice per year.
For the last two years, there has been limited involvement of state ministries and county health departments (CHDs) in the direct implementation of emergency nutrition activities in the context of South Sudan. Contributing factors include insecurity in some of the locations, limited number of staff trained on nutrition and limited logistics capacity. However, following the development of the new CMAM guideline in 2017, a total of 251 participants in nine former states, including government staff, were trained on SAM and MAM management.
Challenges
Transparency and AAP are still a challenge in all five elements/commitments (leadership/ governance; transparency; feedback and complaints;, participation; and design, monitoring and evaluation). The cluster, through the QAAP TWG, has requested all partners to include the minimum six indicators agreed to be monitored by the cluster on AAP. Some partners are only active in the cluster during HRP preparation and the South Sudan humanitarian fund (SSHF) funding process, which limits engagement and accountability. Late funding from some donors has delayed implementation of some of the nutrition projects. In practice, there are PCA/FLA challenges from partners as well as from UNICEF and WFP. Failure to acknowledge gaps during project implementation and a territorial attitude among some of the partners has hampered programming, with incidences of some partners trying to forcefully initiate response in other partners’ operational areas. These are sorted out by the cluster coordination team through tripartite coordination meetings. Linking provision of funding to an emergency threshold undermines the preventative aspects of nutrition responses and encourages late responses, at which point more children will have been affected by acute malnutrition. Some partners raise funding first for areas without consulting the cluster coordination team as to whether there is need/space to engage a new partner. This leads to potential duplication of services and sometimes misunderstanding among the partners involved before the overlap is sorted out by the cluster or local authorities.
Cluster implementation experiences have identified that field visits are a must; independent monitoring of nutrition projects is important to avoid biased reports and complaints of unfairness in some situations. Government involvement at county and community levels in planning, implementation, monitoring and supervision of projects instils ownership. Transparency and openness in engagement with partners on response issues builds trust and confidence – the cluster is the place where issues of overlap or differences can be objectively resolved. Devising an inclusive and transparent strategy for national NGO engagement in humanitarian response, coupled with regular updates on strategy implementation status, might clear misunderstanding and help prevent encroachment into other partner’s operational areas.
Resource monitoring
Funding
The Nutrition Cluster uses two ways of monitoring funding secured for emergency nutrition response: the OCHA FTS and the cluster funding tracking tool. While the OCHA FTS tracks funding for projects in the HRP, the cluster tool tracks financial status from projects both in the HRP and those outside it. Projects outside the HRP include projects funded bilaterally either with funds from partners’ HQs, or development partners who transit to emergency response as the situation evolves, in consultation with their respective donors. This is very important information to the cluster. For example, recent analysis by OCHA SSHF (August 2017) indicated there were no projects outside the FTS, whereas in reality there were 14 projects (including five MSF agencies)1 not reflected in the HRP. The cluster financial tracking tool is usually updated once per quarter or twice per year.
Supplies
Core supplies are procured and delivered to partners by UNICEF and WFP. Regular update of core supplies pipeline is provided by WFP and UNICEF on a monthly basis to all Nutrition Cluster partners during cluster meetings. The Nutrition Cluster also tracks supplies status at site level on a monthly basis for key core pipeline items, including RUSF for TSFP and RUTF for OTP. If any site has stock out, the number of days and reasons for stock out are reported. The cluster coordination team consolidates all the information and presents the summary to Nutrition Cluster partners, WFP and UNICEF. Since this information started being collected in March 2017, the proportion of sites with adequate supplies through the month has ranged from 70 to 83 per cent for TSFP sites and 77 to 92 per cent for OTP sites. Where necessary, the cluster seeks clarification from WFP, UNICEF or the partner concerned. Information on status of partners’ own supplies is not regularly received. The cluster requested partners to provide this information in 2015 and in 2016; none did so, despite having procured buffer stock in case of shortfall/delayed delivery. The cluster is pursuing partners’ own supply reporting in 2017.
Human resource capacity
The Nutrition Cluster drafted a tool in 2015 for partners’ capacity mapping. This tracks the number of existing staff in each organisation and how many have been trained or need to be trained on SMART surveys, CMAM, IYCF and coordination twice per year. About 57 per cent of 1,51 target staff had been trained by end of September 2017. The Nutrition Cluster coordination team also follows up on recommendations by different TWGs (CMAM, MIYCN, NIWG and QAAP) on their capacity-building action plans. For example, the CMAM TWG released its capacity-building plan for 2017 for the new CMAM guideline that was implemented by MoH/UNICEF/WFP/SCI in collaboration with the Nutrition Cluster coordination team. The Nutrition Cluster requests partners’ profiles when joining the cluster for the first time. This provides an understanding of partners’ capacity and guides them on which forthcoming training they should attend/participate in to sharpen and broaden their understanding so that they are on the same level as other organisations.
Challenges
Not all partners provide funding information to the cluster (approximately 75 per cent provide this information sometimes), which hampers timely understanding of cluster funding status and coordination in general. Some partners are also hesitant to provide their own supply information to the cluster, making it difficult to calculate/understand overall supplies and coordinate in a timely way regarding shortfalls/excesses. This is coupled with interruption of supply pipelines due to insecurity and transportation challenges, plus limited supply storage and safety among partners at site level. Some partners request supplies based on FLA/PCA instead of the real needs of beneficiaries on the ground, leading to excess supplies in some instances. High staff turnover leads to inadequate implementation capacity among some of the partners.
Open and honest discussions with cluster partners and donors increases trust and credibility of the cluster coordination team. Continuous capacity building is inevitable in an emergency context that is characterised by high staff turnover, as is the case in South Sudan. Monitoring supplies status at site level has helped in understanding the challenges and systematically devising actions to address them.
Response monitoring and accountability mechanisms
As part of the Nutrition Cluster response plan development process, the cluster coordination team recommends minimum key indicators that should be monitored and reported/updated monthly as per OCHA guidance. The indicators are then reviewed by the SAG, then discussed and approved by partners. Monthly programme reports (TFP (stabilisation centre (SC) and OTP), TSFP, IYCF, BSFP) are submitted by partners either through the nutrition information system (NIS) or 5Ws tools. The reports/updates are consolidated by the cluster coordination team on a monthly basis and an update is provided to all Nutrition Cluster partners during the fortnightly cluster meetings.
Field monitoring and supervision visits are conducted regularly by UNICEF, WFP and MoH or jointly with either the cluster or donor field visits. Partners also conduct their own monitoring and supervisions; however, the Nutrition Cluster is not updated on these.
The Nutrition Cluster, through the QAAP TWG, in collaboration with the Global Tech Rapid Response Team (Tech RRT), with funding from the United States Agency for International Development/Office of the United States Foreign Disaster Assistance (USAID/OFDA), is now engaging Tech RRT technical support in areas on IYCF and monitoring of nutrition projects implemented by partners. With respect to the monitoring, a random selection of projects will be monitored, technical support provided in the field and an action plan for improving quality of services prepared and monitored by the cluster. This is a new initiative which was expected to commence in January 2018.
Accountability
PCAs/FLAs keep partners accountable for delivering on agreed interventions and monitoring and supervision activities, including capacity building of staff and improvement of infrastructures where appropriate. The Nutrition Cluster is generally updated and involved in discussions regarding performance and accountability issues emanating from either WFP or UNICEF monitoring and supervision visits. In a number of instances, the Nutrition Cluster has organised meetings to find solutions on accountability-related issues identified during the field visits conducted either by UNICEF or WFP.
To ensure that AAP is uniformly implemented/adopted by all Nutrition Cluster partners, partners were oriented on the Nutrition Cluster framework on accountability, which was distributed to all Nutrition Cluster partners during the first half of 2016. However, it was not implemented or reflected in partners’ projects until the QAAP TWG was formed in early 2017. Among other things, the QAAP TWG recommends a minimum of six indicators that should be monitored by the Nutrition Cluster coordination team in four elements of AAP (transparency and communication, monitoring and evaluation, complaints and feedback mechanisms, planning and implementation). The six indicators are currently reflected in most of the partners’ projects, especially those reviewed by the cluster peer review team. The six indicators have also been shared with donors, who are encouraged to reflect them in their respective bilateral projects.
Challenges
Reliability of some monthly reports in terms of performance indicators and beneficiaries in the programme is a challenge. In some situations, there are questions regarding ethical and transparency issues among some of the partners in terms of adhering to agreed guidelines and standards on management of acute malnutrition. Some stakeholders only include SAM/GAM prevalence, crude and under-five mortality rate as the nutrition indicators to describe the nutrition situation of an area/county, which greatly limits interpretation and analysis.
Lessons learned
Joint verification of randomly selected reports/nutrition sites enhances transparency, acknowledgement of gaps and invites joint solutions. Open and honest discussions with cluster partners and donors increases trust and credibility of the cluster coordination team.
Mentoring new partners, especially national NGOs, needs patience, understanding of context and appropriate guidance on how they can be part of the humanitarian community. Increased monitoring and supervision significantly improves quality and performance of emergency nutrition projects. Establishment of quality and AAP with independent monitors/agencies is the best way of monitoring partners’ projects and documenting and sharing best practices within and outside the country.
Reflections on developments over the last 12 months
By the end of the third quarter of 2017, Nutrition Cluster partners implemented nutrition activities in ten former states, in 69 out of 79 counties. The coverage of OTP services increased by 8.5 per cent, from 678 in 2016 to 736 in 2017, while TSFP coverage increased by 40.3 per cent, from 504 to 707, during the same period.
In terms of transparency and accountability, there has been an increase in the number of partners acknowledging their technical gaps and requesting technical support, including paving the way for other partners to take over operational areas.
The funding environment is also changing. Most funding support provided to Nutrition Cluster partners is short-term, ranging from three months (for example, the Rapid Response Fund managed by the International Organization for Migration (IOM)) to 12 months (for example, the SSHF). However, there is now bilateral funding to partners that extends beyond one year, such as the HPF, which has a nutrition component supported by the UK Department for International Development. There are also in-kind donations, especially of core pipeline supplies, most of which are short-term extending to one year.
The way in which WFP, UNICEF and the Nutrition Cluster work together has improved significantly in 2017. For example, review of the WFP and UNICEF 2016/17 joint response plan and development of the 2017/18 plan involved the Nutrition Cluster. A joint monitoring and supervision plan was prepared by the cluster and agreed by both UNICEF and WFP. A high-level quarterly meeting was established between WFP and UNICEF management (representative level) and the Nutrition Cluster to review the implementation of the work plan and support the cluster in areas of need, such as development of contingency and preparedness plans where the cluster was still lagging behind.
There have also been significant improvements in inter-cluster (sector) collaboration. During the famine response in Unity State, for instance, the four clusters (FSL, Health, WASH and Nutrition) developed an integrated response plan. The Nutrition and FSL clusters developed an action plan for implementation of an integrated response plan for prevention of famine. The action plan was discussed and approved by the Nutrition and FSL cluster partners. A number of collaboration activities were also carried out with the Health Cluster. For example, the Health Cluster trained Nutrition Cluster partners on rapid testing and treatment of malaria in OTP sites; the first time such a collaboration was implemented at scale. Nutrition Cluster (UNICEF) agreed with Health Cluster (WHO) to procure SC kits and necessary funds were allocated to the Health Cluster rather than the Nutrition Cluster. The WASH and Health Clusters agreed to implement the guidance provided by the Nutrition Cluster on treatment of children with SAM and cholera.
Conclusions
The experiences detailed in this article reflect what partnership and accountability look like on the ground during implementation of core cluster functions. Considerable strides have been made, despite continuing conflicts since 2013 and many ongoing challenges. One of the key lessons learned is that partnership and accountability are products of transparency in all aspects of the implementation of the humanitarian project cycle, including trust; as is open feedback/dialogue among all the stakeholders.
High staff turnover, questionable ethical behaviour and competition for operational opportunities/space by some of the implementing partners stifle efforts to improve partnership and accountability. More work and efforts are still needed for sustained improvement in partnership and accountability through continuous capacity building, monitoring and awareness raising and ensuring that lessons learned are used to improve ongoing and future emergency nutrition programming. One task could be to devise a mechanism to document good partnership and accountability elements and factors contributing to their successes or hindrance in all projects implemented by partners, so that the positive elements can be emulated by other stakeholders.
For more information, contact: Isaack Manyama
Endnotes
1This is based on the Nutrition Cluster’s understanding of MSF sister agencies nutrition responses. The Nutrition Cluster does not track funding status of MSF sister agencies.


