GOAL’s experiences of management of at-risk mothers and infants (MAMI) programming in Ethiopia
This article has been updated since the original version was published in March 2020.
By Alice Burrell and Hatty Barthorp
Alice Burrell has been working in humanitarian nutrition for the past five years, with experience across Asia, Africa, the Middle East and Europe, mostly in refugee or internal-displacement contexts. Alice has worked with GOAL, Action Against Hunger and Save the Children UK and is currently an Emergency Nutrition Advisor – MAMI at Save the Children US.
Hatty Barthorp is a Global Nutrition Advisor at GOAL’s headquarters. She has been working on emergency, transitional and development programmes for 18 years.
The authors would like to thank the DropBox Foundation for funding the progressive innovations during 2019 in collaboration with the Bureau of Population, Refugee and Migration (BPRM) – United States Department of State, the United Nations High Commission for Refugees (UNHCR) and the United Nations Children’s Fund (UNICEF).
Location: Ethiopia
What we know: Management of ‘at risk’ mothers and infants under six months old (MAMI) is an increasing priority for programmers; there are gaps in evidence in how to identify and manage cases in different contexts.
What this article adds: In 2014, GOAL integrated the MAMI approach into its nutrition programme in two refugee camps in Gambella, Ethiopia, using a locally adapted version of the C-MAMI tool. Enrolment and discharge criteria include anthropometric, clinical, feeding and maternal factors. Community screening is undertaken by community outreach agents using simple referral criteria and thorough monthly screening by counsellors at the nutrition centre. A reversible MAMI mid-upper arm circumference (MUAC) tape has been designed by GOAL to support easy identification of at-risk infants under six months old and is being used to trial MUAC thresholds to identify infants in this age group. Defaulter rate was high due to population mobility; among those who remained in the camp, cure rate was 71%. Qualitative feedback from community members, beneficiary mothers and staff reveals that the programme is highly valued; staff suggested that simplification of the C-MAMI tool would aid implementation. Planned programme innovations by GOAL include the use of educational breastfeeding videos in counselling and digital data gathering and analytics. In line with global thinking on the MAMI approach, the programme also plans to transition from an admission/discharge model to enrolment/de-escalated follow-up to six months, recognising the ongoing vulnerability of infants identified as ‘at risk’.
Background
The GOAL programme in Ethiopia spans the child protection; health; nutrition; water, sanitation and hygiene (WASH) and livelihoods sectors. GOAL first became operational in Ethiopia in 1984, following the period of famine, and was registered as a non-governmental Organisation (NGO) in 1991. It has played a significant role in the response to the refugee influx into Ethiopia since 2011, when it began supporting Somali refugees in Dollo Ado camp. Today, GOAL Ethiopia provides nutrition services for refugees in a number of contexts in the country, including South Sudanese refugees in two camps in Gambella (Terkidi and Kule). Here, GOAL runs a nutrition programme that includes community-based management of acute malnutrition (CMAM) and infant and young child feeding (IYCF). In response to the high number of vulnerable mothers and infants in Terkidi and Kule camps,1 in 2014 GOAL integrated the management of ‘at-risk’ mothers and infants under six months of age (MAMI) approach into its nutrition programmes. Originally, MAMI was seen by the GOAL team as an adjunct to community-based management of acute malnutrition model (CMAM) programmes; however, it is now recognised as both a preventative and curative approach.
Experiences of implementing the MAMI approach
The MAMI programme in Gambella uses the C-MAMI V2.0 tool as a key resource to guide programming (see Box 1). The tool’s programme cards have been adapted and a MEAL (monitoring, evaluation, accountability and learning) toolkit has been developed to suit the specific context. This includes an electronic database with digital data entry for enrolment and management, a screening register, enrolment register, beneficiary monitoring cards and ‘ration’ cards. Figure 1 shows the flow of the programme and the monitoring and evaluation tools that are used at each stage of the programme. Figure 2 shows how MAMI services are located within the wider GOAL nutrition programme in Gambella. MAMI services are offered within the IYCF space, with close links to the blanket supplementary feeding programme (BSFP) and the stabilisation centre (SC) when complications are identified.
Box 1: The C-MAMI tool
The C-MAMI tool is a resource that provides a health worker with a pathway and supporting content to assess, identify/classify and manage at-risk mothers and infants under six months old who are nutritionally vulnerable in the community. It was developed as a first step to help fill a gap in programming guidance on community case management of uncomplicated cases. The tool draws on and complements existing national and international guidance and protocols and is modelled on the integrated management of childhood illness (IMCI) approach.
Figure 1: Programme flow with monitoring and evaluation tools used at each stage
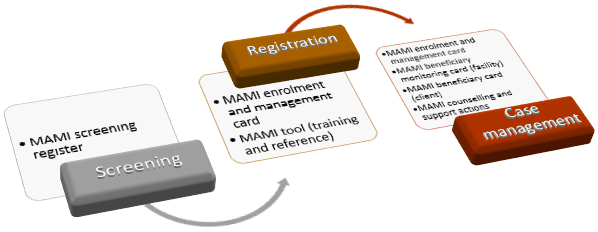
The MAMI enrolment and management card has been adapted from CMAMI V2.0 tool versions.
Figure 2: Services available at GOAL nutrition sites in refugee camps in Gambella, Ethiopia
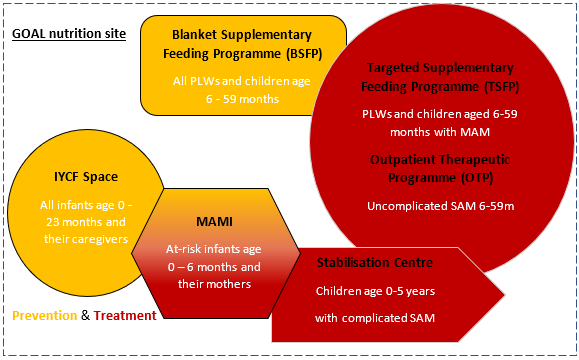
IYCF = infant and young child feeding; PLWs = pregnant and lactating women; MAM = moderate acute malnutrition; SAM = severe acute malnutrition; MAMI = management of ‘at risk’ mothers and infants under six months of age
Identifying at-risk mothers and infants
Enrolment criteria
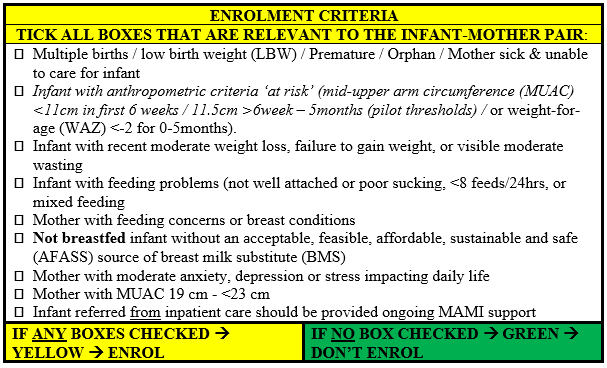
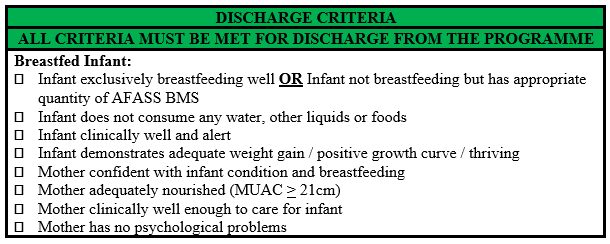
When the programme first began, at-risk infants were identified using only anthropometric criteria. However, anthropometry for this age group has limitations and infant feeding and maternal factors are also essential in identifying risk in the age group. Therefore, in line with the updated version (V2.0) of the C-MAMI tool, enrolment and discharge criteria used in the GOAL Gambella programme were expanded in June 2019 and now encompass a broader set of clinical, feeding and maternal factors (see Boxes 2 and 3).
Box 2: Enrolment criteria for the GOAL MAMI programme in Gambella from June 2019
Box 3: Discharge criteria for the GOAL MAMI programme in Gambella from June 2019
Monthly screenings as per enrolment criteria are currently conducted for all mothers and their infants under six months of age at each nutrition site. Finding that, in practice, some health workers were applying a more thorough assessment of admission criteria than others, simple screening registers were developed that clearly list each criterion to ensure that they are all systematically reviewed. This maximises case identification. In December 2019, to improve case identification and geographical reach further, GOAL trained community outreach agents (COAs) on MAMI community screening and referral to equip them to make referrals for assessment. The training followed an ‘A, B, C, D’ format, checking Anthropometry (mid-upper arm circumference (MUAC) and oedema); Breastfeeding status and challenges; Clinical illness of infant and mother; and Depression, anxiety or stress of the mother.
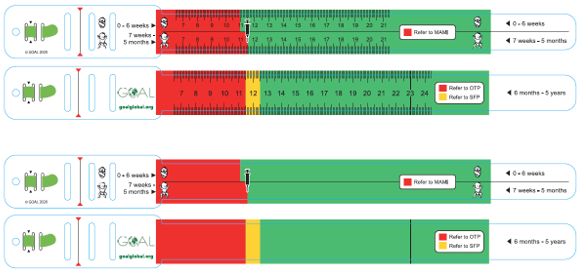
MAMI-MUAC
International validated thresholds for MUAC to identify at-risk infants under six months have not yet been agreed. As a result, this age group has not been included in community-level nutrition screenings that rely on MUAC (Lelijveld et al, 2017). Given this and the significant limitations of using weight-for-length in this age group and operational setting, GOAL Ethiopia is currently trialing the use of two MUAC thresholds to identify nutritional risk in infants under six months and has designed a reversible MAMI-MUAC tape to support easy identification. One side of the tape is used to identify older children (6-59 months of age) and mothers with nutritional risk using standard international cut-offs, and the reverse is used to identify infants under six months with nutritional risk. Thresholds for infants were selected based on existing evidence by Mwangome et al (2017), as follows:
- <110mm for infants aged 0 to 6 weeks of age.
- <115mm for infants aged >6 weeks to 5 completed months of age.
Age groups for thresholds were selected to coincide with first vaccinations at six weeks, which provides a good marker for families and reinforces vaccine schedules. MAMI-MUAC tapes were designed with community input and testing.
Figure 3 shows the final MAMI-MUAC tape designs. Features include:
- A broad 25mm tape that reduces the effect of over-tensioning.
- A three-slot ‘buckle’ that reduces measurement error (Grant et al, 2018).
- A reversible tape to include infants age 0 to five months, infants age 6 to 59 months and a marker for maternal risk at 23cm.
- An enumerated version for health workers and a non-enumerated version for community screening.
Figure 3: MAMI-MUAC tape design: Enumerated (top) for use with trained health workers and non-enumerated (bottom) for use in the community
Programme outcomes
From May 2019 to January 2020, the programme enrolled 114 infants, 110 of whom were with their mothers and four of whom were orphaned and with a caregiver. Figure 4 shows the enrolment criteria that were met for these MAMI enrolments. Criteria are not mutually exclusive and numerous criteria can be met for one mother-infant dyad. Figure 5 shows the age in months and the sex of the 114 infants enrolled, revealing that the most common age at enrolment is 0 months (newborn), followed by the younger age groups.
The average length of stay in the MAMI programme is 44 days. This ranges from 33 days in Terkidi site 1 to 58 days in Kule site 2. The average weight gain is 0.73 g/kg/day and average MUAC gain during programme enrolment is 1.1 mm (Table 1).
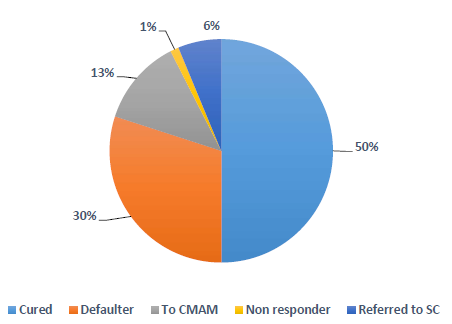
Figure 6 shows the outcomes of the 83 mother-infant dyads discharged from the MAMI programme in the study period (i.e. cure, default, transfer to stabilisation centre, transfer to CMAM programme, death). No baseline data on outcomes without treatment is available. Recorded cure rate (50%) was affected by a high default rate (30%), experienced across all GOAL nutrition programmes due to the considerable fluidity of the camp population as families cross the border to and from South Sudan, as well as between the camp and host communities where many have relatives. Among the 56 who remained in the camp until discharge, cure rate was 71.0%.
Figure 4: Enrolment profile of the GOAL MAMI programme in Gambella (114 infants and 100 mothers)
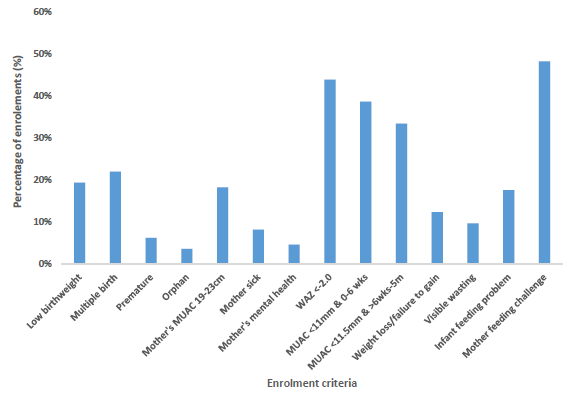
Figure 5: Age and sex of the enrolments to the MAMI programme, May 2019 to January 2020
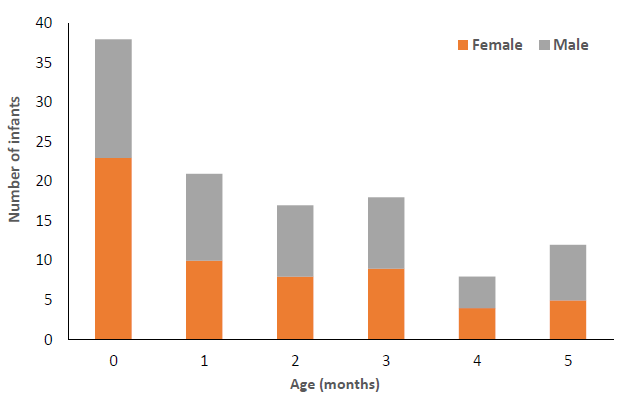
Table 1: MAMI programme outcomes at discharge by nutrition site
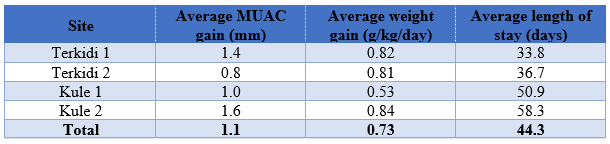
Figure 6: Outcomes at discharge of 83 discharged mother-infant dyads
Perceptions and experiences of the MAMI programme
In October 2019, GOAL conducted a qualitative survey on the utility and acceptability of the MAMI programme among Gambella refugees. The survey included focus groups with community members and interviews with MAMI programme staff. Results show that the purpose of the service is well understood by both health workers and MAMI beneficiaries. Both groups cited improved learning as the main focus of the programme (including in breastfeeding and care practices for the infant and mother), as well as to both prevent and treat malnutrition. Health workers and beneficiaries had a very positive perception of the programme, with both groups describing the benefits of the service as improved health and nutritional status (recognised as weight gain) and improved breastfeeding and care practices. There was, however, an incorrect perception that ‘food provision’ was part of the service. This can be explained by the fact that MAMI support, in this context, is a nested activity within the wider CMAM and BSFP programmes, where beneficiaries do receive food commodities (such as Plumpy’Nut and basic medicines in the case of CMAM, and fortified blended flours and micronutrients in the BSFP). The most significant motivator conveyed by both groups was the perceived value of support provided by the programme that resulted in improved knowledge and practices, and demonstrated in the positive impact they witnessed on the health and wellbeing of their babies. A smaller proportion of those interviewed in both groups liked being able to see the growth of infants by plotting progress against growth curves.
In terms of barriers and challenges, almost all MAMI beneficiaries noted that workload of the caregiver made it problematic to attend the programme. Participation in the MAMI programme requires weekly visits to the nutrition centre, where mothers attend MAMI follow-up and the BSFP and, if they or their older children are enrolled, they may also attend a targeted supplementary feeding programme (TSFP) and/or OTP. This may take anything from one hour up to half a day, depending on caseloads and the number of services the family is enrolled in. The four nutrition sites are spread between the two camps to optimise access, with a maximum walk time of 30 minutes each way. Comparing this to a non-camp, rural setting, many households outside the immediate catchment of a health facility would walk for a number of hours to access services, which requires a greater perceived ‘cost’. Multiple commodity revisions of the general food ration in the last few years have required families to access income and/or food from other sources as a supplement, creating an extra time-burden. The lack of tangible assets or goods received in the MAMI programme (such as soap, jerry cans, kitchen utensils and bed nets) was also flagged by the beneficiary group as being a negative element of the service. But, given that this is a largely aid-dependent population, their desire and/or expectation for physical assets are likely to be greater than would be encountered in other contexts.
Staff were interviewed about the utility of the C-MAMI tool. Results showed that most staff were not using the tool directly for assessment but rather as a reference guide, due to its length. Staff were instead using either the enrolment and management card or the GOAL digital data tool (which exactly mirrors the enrolment and management card) as a form of screening, as well as enrolment. Staff did report, however, using the counselling support actions and/or accompanying counselling cards as intended. Staff requested that the C-MAMI tool be simplified and shortened to enable its use in contexts where time for assessment and enrolment is limited.
MAMI innovations through programming
Several innovations have been made by the programme in delivering the MAMI approach.
Breastfeeding educational videos as a counselling tool
The breastfeeding educational videos for mothers developed by Global Health Media (GHM) Project2 have been translated to Nuer language for use in the MAMI (and IYCF) programmes. The videos will be downloaded onto tablets and used by health workers with the aim of improving beneficiary engagement and behaviour change. The videos will be trialled in Gambella in early 2020 and a study will be conducted alongside to measure the impact of their use on breastfeeding knowledge and behaviours compared to traditional methods of didactic counselling and education.
Digital data gathering
In May 2019, GOAL switched to digital data gathering in the MAMI programme. Forms directly reflecting the paper-based versions were created on CommCare and downloaded to handheld tablets for health workers to directly enter enrolment and follow-up data. This supports more timely data collection and improves data quality, using skip logic to reduce missing, invalid or inaccurate data entries, auto calculate for certain data such as age and weight gain, and adding limitations to the values entered. This method also allows for easy tracking of individuals over time with case management functions.
Additional data values have also been added, including: maternal age, maternal height, moderate maternal mental health issues, recent moderate weight loss/failure to gain weight of infant, visible moderate wasting of infant, and an expanded feeding section, including mixed feeding, identification of breast conditions, attachment and suckling status, inadequate milk/other feeding issues. These will be used to assess potential risk factors for infant malnutrition. From July 2019, GOAL began to collect longitudinal data at 1, 2, 6 and 12 months post-discharge to enable assessment of future risk of relapse with associated causes, risk of death, at what age, how long post-discharge and anthropometric outcomes.
Analytics dashboard
GOAL has been using PowerBI to develop automated dashboards to compile project data and perform real-time analytics for project staff and to help identify quality issues which, in conjunction with real-time digital beneficiary feedback, supports adaptive programme management.
Next steps
Research findings from the qualitative study will feed into an internal action plan to improve the acceptability and quality of the MAMI programme in Gambella. Actions to improve cure rates include having a dedicated person to improve technical capacity of staff in terms of counselling and programme flow, and case reviews of infants who remain in the programme for longer periods to understand barriers to management. Findings relevant to the ongoing development of the C-MAMI tool will be shared with the MAMI Special Interest Group (SIG)3 and other relevant platforms. Digital data collection will continue and, once a sufficient sample size has been achieved, an analysis of programme data will be conducted to assess potential risk factors for infant malnutrition and impact of the MAMI programme, including the longitudinal outcomes of infants after discharge. Although currently the programme in Gambella uses a set of admission criteria and corresponding discharge criteria, GOAL recognises that this needs to be transitioned to enrolment with de-escalated follow-up to six months, rather than discharge on attaining anthropometric/non-anthropometric thresholds, due to the ongoing vulnerability of such small infants who have been identified as ‘at risk’. This will be reflected in future iterations of this programme.
GOAL is committed to building the evidence base for MAMI programming, with practical operational experiences and learning feeding into the C-MAMI tool update4 (now underway) and, more broadly, into development of the MAMI approach.
For more information, please contact Hatty Barthorp.
References
Grant et al (2018). Comparing performance of mothers using simplified mid-upper arm circumference (MUAC) classification devices with an improved MUAC insertion tape in Isiolo County, Kenya. Archives of Public Health. February 2018.
Lelijveld N, Kerac M, McGrath M, Mwangome M, Berkley JA (2017). A review of methods to detect cases of severely malnourished infants less than 6 months for their admission into therapeutic care. ENN. May 2017
Mwangome et al (2017). Diagnostic criteria for severe acute malnutrition among infants aged under 6 mo. AJCN. April 2017.
UNHCR, Ethiopia Comprehensive Registration Data (Return Intention Profile). November 2019. Accessed at https://data2.unhcr.org/en/documents/download/72513
1 Current estimated populations of 61,918 and 43,426 persons and 624 and 571 infants under six months of age respectively (UNHCR, 2019).
2 https://globalhealthmedia.org/videos/breastfeeding/


