The link between foetal and childhood nutrition and adult non-communicable disease: lessons from birth cohort studies in India
Research summary1
Location: India
What we know: Non-communicable diseases (NCDs) are rising in prevalence globally and they particularly affect younger and thinner people in South Asia, most likely due to poor early life nutrition.
What this article adds: Several cohort studies in India over the past 20 years have provided evidence of the links between early life nutrition and the risk of NCDs in adulthood. Birth cohorts have established links between prenatal undernutrition (often defined by low birth weight (LBW)) and later life obesity, diabetes and cardiovascular disease. Risks are especially high in babies who are born small and then gain weight in childhood, even if they do not become overweight or obese. Mothers with gestational diabetes, malnutrition (both over- and under-nutrition), a heavier physical workload, low intakes of micronutrient-rich food such as green leafy vegetables, dairy products and fruit and deficiencies in folate, vitamin C and B12 are all at higher risk of having LBW babies. More evidence on effective interventions to break this cycle is needed; interventions targeting adolescents to improve their nutritional status before they become pregnant may be effective.
Introduction
Cardiovascular disease (CVD) is the leading cause of death in India. Since the 1960s, the prevalence of CVD in India has been rising sharply, where it is more deadly and affects younger and thinner adults than in other parts of the world. Although obesity, a major risk factor for CVD, is not as high in India as in other parts of the world, its prevalence there is rising and other non-communicable diseases (NCDs) such as hypertension, type 2 diabetes (T2DM) and dyslipidaemia are common. Elucidating the reason behind this higher and deadly prevalence of NCDs in India is of huge public health importance.
Several Indian cohort studies have taken place over the past 20 years which have helped shine light on the causes of adult NCDs, most notably the influence of prenatal and early life nutrition. Since Barker’s “foetal programming hypothesis” in the 1970s and the subsequent creation of the developmental origins of health and disease (DOHaD) concept, Indian researchers were quick to recognise the potential relevance of these ideas to India’s NCD epidemic. This article provides a summary of some influential Indian cohort studies and their programme and policy implications for Southeast Asia.
Prenatal nutrition and adult health
A number of birth cohorts in India have found an association between prenatal nutritional environment and risk factors for non-communicable diseases (NCDs). Low birth weight (LBW) is used as the indicator for sub-optimal foetal nutrition; Bavdekar et al., (1990) found lower birth weight in a cohort of children in Pune to be associated with higher blood pressure, higher plasma glucose and cholesterol concentrations, insulin resistance and central adiposity in childhood. They found the highest risk was in children who had “caught up” and become heavier than average by eight years of age. Rapid weight gain, or “starting small and becoming big” is now a well-established risk factor for later cardio-metabolic disease. Further follow-up of the Pune cohort at 21 years found similar results (Joshi 2014).
Another study, which used hospital birth records since 1934 in Mysore and tracked the adults by house-to-house survey in order to assess long-term outcomes, found similar results (Krishna 2015). As well as an association between LBW and a higher risk of cardiovascular disease (CVD), it also found something new: babies who were fatter at birth, or those with larger mothers, had a greater risk of developing type 2 diabetes (T2DM). Based on evidence from other studies that foetal exposure to gestational diabetes increases risk of later life T2DM, this likely explains these results. Gestational diabetes affects up to 20% of urban Indian women so breaking this intergenerational cycling is imperative for improving population health.
Prospective cohorts including the Pune Maternal Nutrition Study (PMNS) (Rao 2001) and the Parthenon Birth Cohort (Krishnaveni 2015) have also provided further important insights into the connection between prenatal nutrition and later adult health and have identified potentially modifiable risk factors during pregnancy. These studies have identified a particularly risky phenotype which seems to be especially prevalent in south east Asian populations called “thin-fat”; these babies are small in all dimensions and have low levels of fat-free tissue (such as muscle) but normal levels of subcutaneous fat. Hence their fat:muscle ratio is a lot higher than most newborns.
Maternal factors associated with smaller newborn size included smaller body size (pre-pregnant height, body mass index, skin folds and arm circumference), a heavier physical workload, low intakes of micronutrient-rich food such as green leafy vegetables, dairy products and fruit, lower blood levels of vitamin C and folate and higher levels of homocysteine (indicative of vitamin B12 deficiency, present in 70% of mothers). Maternal vitamin D insufficiency and low vitamin B12 concentrations are associated with lower muscle mass, higher adiposity and higher insulin resistance in their children. Low vitamin B12 in mothers is also a risk factor for gestational diabetes which we know leads to an increased risk of obesity and NCDs for the exposed offspring.
Low B12 concentrations are known to be common in lots of Indian populations and may be an important area for intervention, the main cause being low dietary intake due to a lack of meat, fish, eggs and diary products. The PMNS cohort has now transitioned into a vitamin B12 intervention study (ongoing) where adolescent cohort members are receiving supplementation and B12 levels and later cardiometabolic outcomes will be assessed in their offspring. If successful, this could have important implications for lifelong health and productivity across Southeast Asia.
Two other intervention studies have also focused on pre-conception nutrition in India. The Mumbai Maternal Nutrition Project (MMNP or “Project SARAS”) provided a daily micronutrient-rich snack in order to improve diet quality and this successfully resulted in a 24% reduction in LBW and an almost 50% reduction in gestational diabetes. The other study, “EINSTEIN”, started in 2018 as part of the multi-country HeLTI family of studies (Healthy Life Trajectories Initiative), includes multi-faceted interventions (nutrition, sanitation and hygiene, environmental and mental health interventions) in a rural South Indian population (ongoing). Interventions later in pregnancy are unlikely to influence the developmental origins of health and disease (DOHaD) effect since they miss foetal organogenesis and placental development, both of which are thought to play a mediating role in foetal programming.
Infant and young child nutrition and adult health
Besides prenatal nutrition, nutrition in infancy, childhood and adulthood are also important in relation to non-communicable disease (NCD) risk. Two large Indian cohorts, the New Delhi and Vellore birth cohorts, have shown in greater depth the risk of “small becoming big” (Bhargava 2018; Antonisamy 2009). They have found that adults (average age, 29 years) with type 2 diabetes (T2DM) were generally born smaller and thinner than those who did not develop T2DM, gained weight quickly in late childhood to catch-up their BMI and then gained further weight in adulthood to exceed the body mass index (BMI) of those without T2DM. Those with T2DM were still thin by international standards but they had gained more weight, more rapidly, than non-T2DM adults in their community.
Intervention in this area is not simple. It is undoubtedly important to prevent and treat childhood obesity but this alone will not prevent the majority of future cases of T2DM in India because many Indian children are born small and catch-up. The challenge is in identifying the low birth weight (LBW) children crossing the BMI centile lines; the New Delhi birth cohort group has published centile charts to detect this growth pattern (Sachdev 2009). Even once identified, high-quality intervention studies in Indian children have shown that it is not easy to prevent BMI gain (Bhave 2016). Moreover, preventing BMI gain among children who were under-nourished in utero, and whose BMI remains well below international norms, is questionable. Preventing the low birth weight in the first place is therefore perhaps the more desirable path for intervention.
Implications for policy and programmes
These studies have taught us that maternal and child nutrition are very important driving factors for lifelong health and the health of the next generation. In Southeast Asia, this is especially pertinent due to the dangerous combination of very high low birth weight (LBW) rates and transitioning diets. Perhaps due to the severity of foetal undernutrition, it appears to take very little transition and only a subtle increase in childhood adiposity to produce these metabolic changes and subsequent non-communicable diseases (NCDs) in this context which, in turn, leads to problems in the next generation. The cycle of undernutrition, subsequent subtle weight gain and the resultant NCDs is depicted in Figure 1.
Figure 1: Diagram depicting the linking cycles of undernutrition and NCDs
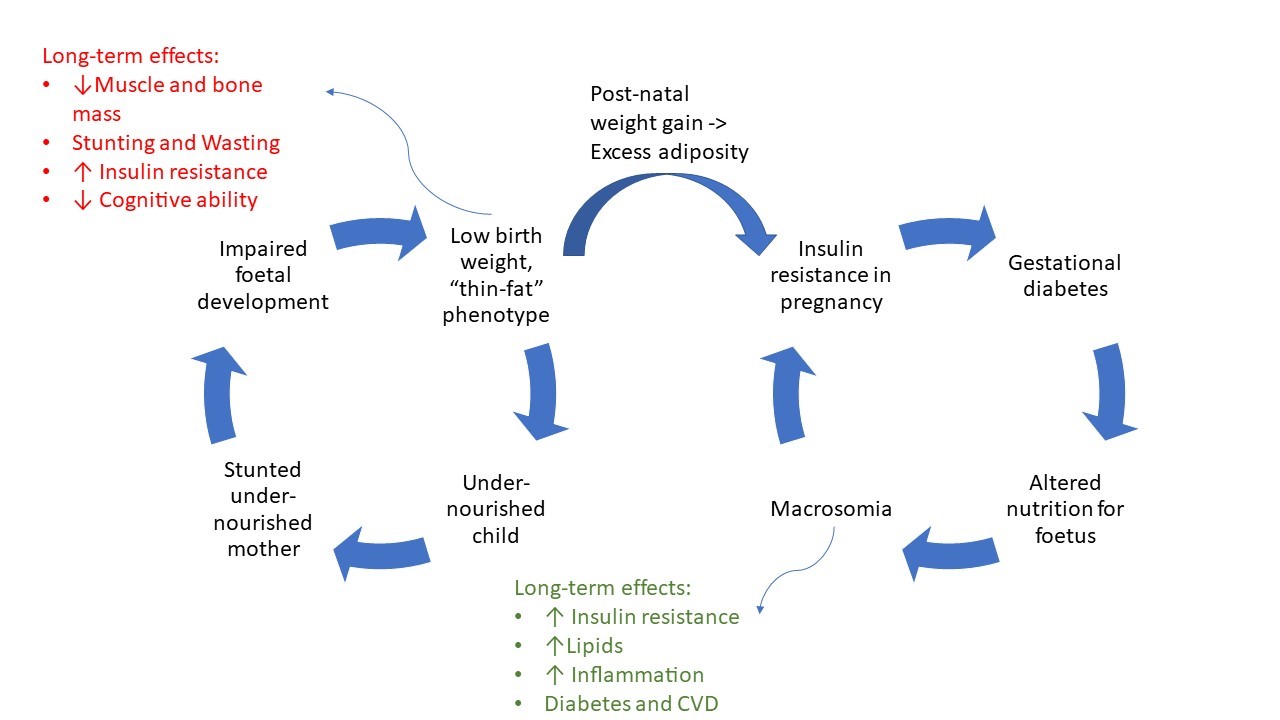
Attempts should be made to break these cycles at several points by improving maternal and infant nutrition and preventing child wasting, stunting and excess body mass index gain. Practitioners and policymakers must recognise that newborn and infant underweight is a risk factor for later NCDs, not just overweight. More evidence is needed to understand exactly what interventions work best but, in the meantime, doubling our efforts to prevent and effectively treat childhood wasting and stunting and focusing on good maternal and adolescent nutrition will not only help that individual survive and thrive but may also help the subsequent generation from falling into the same trap.
Endnotes
1 Fall, CHD. (2018) Nutrition in Fetal Life and Childhood and Its Linkage with Adult Non-Communicable Disease: Lessons from Birth Cohort Studies in India. Proc Indian Natn Sci Acad 84 No. 4 December 2018 pp. 881-889
References
Antonisamy B, Raghupathy P, Christopher S, Richard J, Rao P S S, Barker D J P and Fall C H D (2009). Cohort profile: The 1969-73 Vellore Birth Cohort Study Int J Epidemiol 38 663-9
Bavdekar A, Yajnik C S, Fall C H D, Bapat S, Pandit A N, Deshpande V, Bhave S, Kellingray S D and Joglekar C (1999). The insulin resistance syndrome in eight-year-old Indian children: small at birth, big at 8 years or both? Diabetes 48 2422-9
Bhargava S K (2018). Adult health and human capital; impact of birth weight and childhood growth. Sage Publications India Pvt Ltd, New Delhi
Bhave S, Pandit A, Yeravdekar R, Madkaikar V, Chinchwade T, Shaikh N, Shaikh T, Naik S, Marley-Zagar E and Fall C H D (2016). Effectiveness of a 5-year school-based intervention programme to reduce adiposity and improve fitness and lifestyle in Indian children Arch Dis Child 101 33-41
Fall, CHD. (2018). Nutrition in Fetal Life and Childhood and Its Linkage with Adult Non-Communicable Disease: Lessons from Birth Cohort Studies in India. Proc Indian Natn Sci Acad 84 No. 4 December 2018 pp. 881-889
Joshi S M, Katre P A, Kumaran K, C Joglekar, Osmond C, Bhat D S, Lubree H, Pandit A, Yajnik C S and Fall C H D (2014). Tracking of cardiovascular risk factors from childhood to young adulthood Int J Cardiol 175 176-8
Krishna M, Kumaran K, Veena S R, Krishanveni G V, Karat S C, Cox V, Coakley P J, Kiran N, Stein C E, Paul B D R, Prince M, Osmond C and Fall C H D (2015). Cohort Profile: The 1934-1966 Mysore Birth Records Cohort in South India Int J Epidemiol 44 1833-41
Krishnaveni G V, Veena S R, Hill J C, Karat S C and Fall C H D (2015a). Cohort Profile: Mysore Parthenon Birth Cohort Int J Epidemiol 44 28-36
Rao S, Yajnik C S, Kanade A, Fall C H D, Margetts B M, Jackson A A, Shier R, Joshi S, Rege S, Lubree H and Desai B (2001). Intake of micronutrient-rich foods in rural Indian mothers is associated with the size of their babies at birth J Nutr 131 1217-1224
Sachdev H P S, Osmond C, Fall C H D, Lakshmy R, Ramji S, Dey Biswas S K, Prabhakaran D, Tandon N, Reddy K S, Barker D J P and Bhargava S K (2009). Predicting adult metabolic syndrome from childhood body mass index; follow-up of the New Delhi Birth Cohort Arch Disease Child 94 768-74


