Maternal mid-upper arm circumference: Still relevant to identify adverse birth outcomes in humanitarian contexts?
Lisez cet article en français ici
Sonia Kapil is a former Graduate Researcher at Emory University, Rollins School of Public Health
Mija Ververs is a Senior Associate at the Center for Humanitarian Health, Johns Hopkins Bloomberg School of Public Health
What we know: Maternal mid-upper-arm circumference (MUAC) was found to be a reliable indicator for risk of subsequent low birth weight (LBW) following a comprehensive review of anthropometric indicators in 2013. However, optimal MUAC cut-off thresholds to identify poor birth and maternal outcomes have remained contentious, with different thresholds being recommended.
What this adds: This scoping review analyses evidence after 2012 to determine whether more recent data sheds further light on optimal MUAC cut-off thresholds to identify those at risk of negative outcomes. The findings highlight that a MUAC cut-off threshold of <23 cm is predictive for identifying pregnant women at risk of adverse birth outcomes, particularly LBW.
Background
Establishing a practical anthropometric measurement, with an appropriate cut-off threshold, to identify pregnant women as undernourished in humanitarian settings can assist in the implementation of necessary interventions to avoid unfavourable maternal and birth outcomes. A key gap in maternal nutrition is that there is currently no agreed-upon standard set in the Sphere Handbook that defines maternal acute undernutrition through an optimal, context-specific MUAC cut-off point (Sphere Association, 2018).
In 2013, Médecins Sans Frontières Switzerland undertook an extensive literature review (Ververs et al, 2013) of articles published between January 1995 and September 2012 exploring anthropometric indicators that are able to identify pregnant women as acutely undernourished and at risk for adverse outcomes – including maternal mortality, low birth weight (LBW), intra-uterine growth restriction (IUGR), pre-term birth (PTB), small-for-gestational-age (SGA), and stunting at birth.
The review concluded that maternal MUAC can be used as a reliable indicator of risk of LBW. Maternal MUAC was identified as the preferential indicator, as opposed to body mass index, maternal weight for gestational age, maternal weight gain, or maternal stature. Maternal MUAC has a strong association with birth weight, is a simple measurement to take, particularly in humanitarian contexts, and is independent from gestational age. The proposed conservative cut-off value to enrol pregnant women in nutritional programmes, most frequently supplementary feeding programmes, was a MUAC of <23 cm.
This scoping review aims to analyse studies published after September 2012, specifically focusing on determining the specific MUAC cut-off threshold used to identify adverse birth and maternal outcomes to understand if a MUAC of <23cm should be used rather than a MUAC of <21cm as is used in some humanitarian nutrition programmes.
Methodology
Data were abstracted from a comprehensive literature search conducted primarily in the PubMed and Embase electronic databases on literature published between September 2012 and October 2022. Additional eligible studies were sought after reviewing the reference lists of identified articles. The focus was on MUAC cut-off thresholds to identify risk of adverse birth and/or maternal outcomes (outcomes are listed in Table 1). PRISMA guidelines facilitated the preparation of this research protocol.
Inclusion criteria were: availability in full text, peer reviewed, in English, and focused on adult maternal anthropometry. This review was not specifically restricted to studies conducted in low- and middle-income countries or protracted humanitarian settings.
Since individual studies were not comparable and different approaches were taken for study analyses, a meta-analysis was not conducted. Data were synthesised based on the results of each individual study, and quantitative results were extracted and organised in thematic tables.
Duplicate publications and studies analysing the same study populations for similar outcomes were excluded. Additional exclusions consisted of results involving: twins, triplets, adolescents, substance abuse, anaemia, cigarette smoking, in-vitro fertilisation, drugs and hormones, disease, and obesity. The quality of studies was assessed using an adaptation of the Newcastle-Ottawa Quality Assessment Scale and the Joanna Briggs Institute Critical Appraisal Checklist.
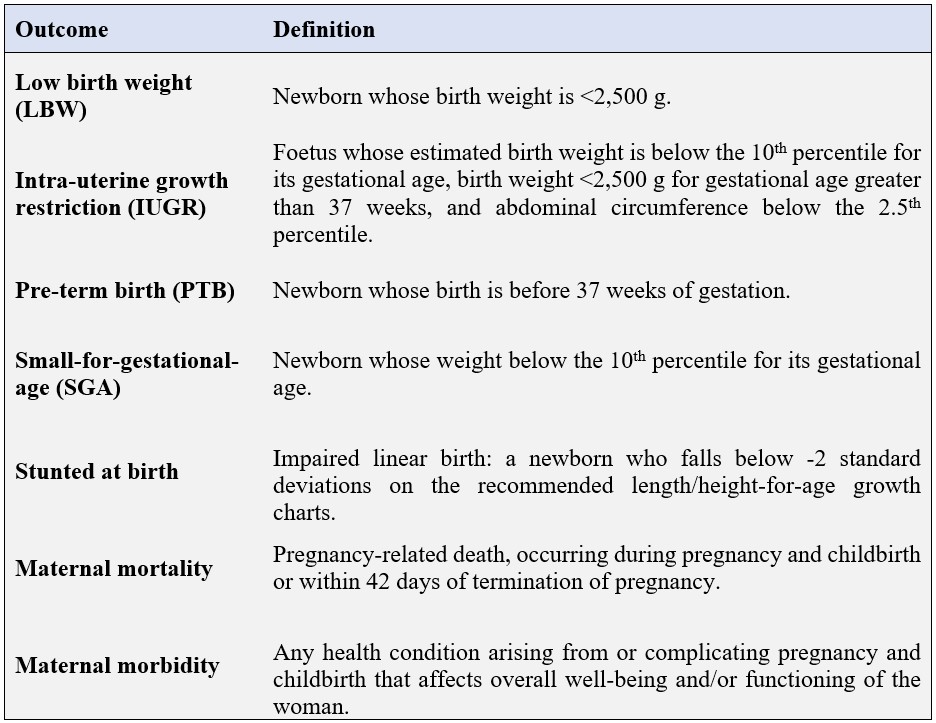
Table 1: Definitions of outcome measures used
Findings
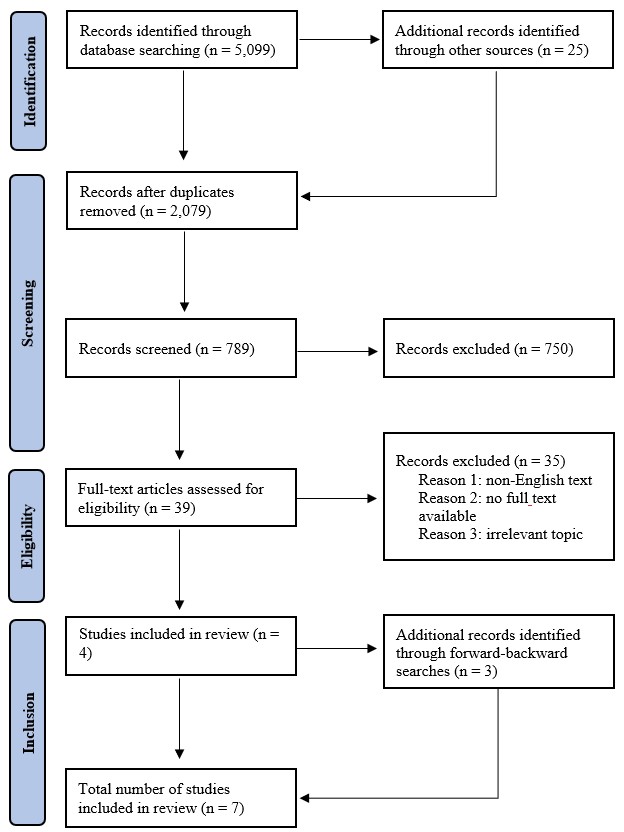
A total of 5,099 articles was initially identified. This was narrowed down to seven suitable articles – which were categorised as either ‘good’ or ’fair’ quality – after multiple stages of review (Figure 1). The studies were conducted in Bangladesh, Cambodia, Ethiopia, Kenya, and India and included women delivering in hospitals (three studies), attending antenatal services (two studies), or part of nutrition interventions (two studies). Three studies were cross-sectional in nature, two were cohort studies, one was a randomised control trial, and one was an unmatched case-control study. According to the adapted quality assessments based on specific study type, all included studies were deemed of good or fair quality, with none being categorised as poor quality.
Figure 1: Article identification and inclusion flowchart
The seven studies (Table 2) demonstrate the specific maternal MUAC cut-off threshold values and the corresponding birth outcomes of LBW, IUGR, SGA, and stunted at birth; sufficient data were not provided on maternal outcomes. Five of these studies indicate a MUAC of <23 cm as strongly predictive for identifying pregnant women as at risk for at least one of these adverse birth outcomes, while one study uses a MUAC cut-off value of ≤ 23 cm and another study used <22 cm. None of these cut-off values are found to be associated with gestational age.
Five of the studies looked at the adverse birth outcome of LBW, with evidence suggesting that a MUAC <23 cm was significantly associated with LBW. One study explored the birth outcome IUGR, and found a MUAC <23 cm measured at delivery to be associated with IUGR. Another study explored SGA and found no significant association with a MUAC <23 cm and SGA. Being stunted at birth was explored in two studies and a MUAC of <23 cm measured during the third trimester was associated with being stunted at birth, although this result was not statistically significant. No studies looked at outcomes such as PTB, maternal morbidity, and maternal mortality.
Table 2: Studies post-September 2012 using maternal MUAC to identify adverse birth outcomes
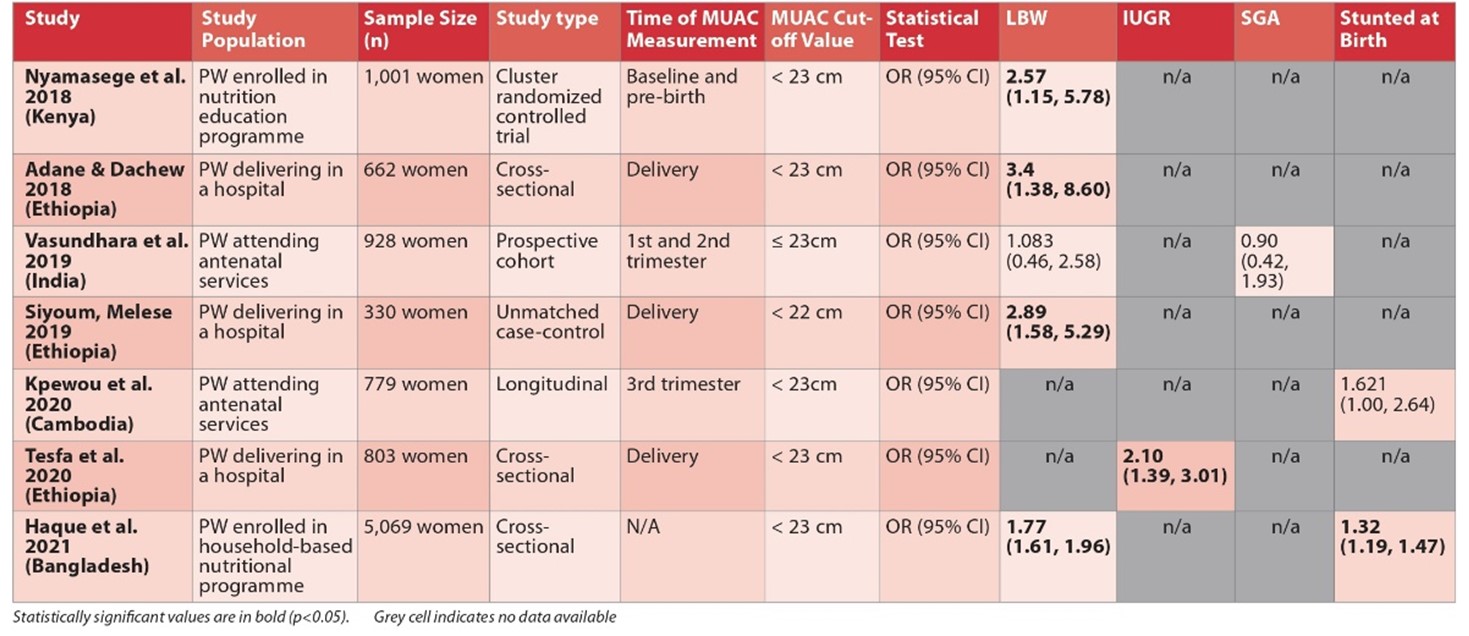
Statistically significant values are in bold (p<0.05)
Discussion
This scoping review explored recently published literature concerning appropriate MUAC cut-off thresholds that can identify pregnant women as undernourished and at risk for adverse birth outcomes. Most of the studies identified utilised a MUAC threshold of <23 cm to identify pregnant women at risk for the following birth outcomes: LBW, IUGR, SGA, and stunted at birth. Results on maternal morbidity and maternal mortality were not sufficiently available.
All studies in Table 2 determined maternal MUAC cut-off values to be independent of gestational age, which is particularly important for humanitarian contexts since gestational age is often unknown for pregnant women in such emergency contexts.
A more recent cross-sectional study from Ethiopia found MUAC <23 cm to be significantly associated with adverse birth outcomes (adjusted OR= 5.93, 95% CI: 3.49, 10.08) (Degno et al, 2021). However, this study was not included in this scoping review because it broadly references ‘adverse birth outcomes’ among study participants, rather than specifying MUAC to be associated with individual birth outcomes.
The study from India (Vasundhara et al, 2019) that used a maternal MUAC cut-off value of ≤ 23 cm did not demonstrate any significant associations with LBW or SGA. Here, the usage of the ‘less than or equal to’ symbol (≤) is unclear as it leaves the specific threshold open for interpretation. Since measurements were not completed in millimetres but rather in centimetres, it is unclear whether values between 23.1 cm and 23.9 cm or 23.4 cm were included in this threshold criteria.
The Sphere Handbook states to consider MUAC <21 cm as an appropriate cut-off for the selection of pregnant women at risk during emergencies (it also states that a MUAC of <23 cm indicates a moderate risk among pregnant women, although moderate risk is not defined (Sphere Association, 2018)). The findings from this review do not support the presented statement, as it has been demonstrated that there is a clear risk of low birthweight found with MUAC <23 cm, with potential associations with other birth outcomes; therefore, we are not in agreement that <21 cm is an appropriate cut-off value to indicate pregnant women as at risk during emergencies.
Though both the previous Médecins Sans Frontières study from 2013 and this scoping review suggest using MUAC <23 cm for pregnant women as an indicator of risk for adverse birth outcomes in humanitarian contexts, we do not have sufficient information to determine if MUAC also can be used as an indicator predicting the potential benefit (e.g., improved foetal growth) of a certain nutritional intervention. Additional information is required on which nutritional interventions with enrolment based on MUAC can sufficiently avert adverse risks.
Lastly, there is a substantial focus in the studies identified on MUAC and adverse infantile or foetal outcomes. However, there is significant need to have more information on adverse maternal outcomes.
Limitations
Limitations of the current literature include the lack of research on maternal outcomes. Additionally, these studies lack focus on humanitarian emergencies or conflict settings, although their findings are still applicable to such contexts. Additionally, only seven studies were included in the final results, meaning that conclusions need to be met with a certain degree of caution. This further highlights the need for more research on this important topic.
Limitations of this scoping review include potential bias due to having only one quality assessment reviewer, lack of comparability between studies due to variations in sample size, methodology, and context, exclusion of studies not available in English that may contain valuable results, and the omission of non-peer-reviewed grey literature, which could have provided noteworthy data.
Recommendation
A recommendation for future research would be to study the enrolment of pregnant women in nutritional interventions based on the use of MUAC <23 cm in efforts to reduce the risk of adverse outcomes. Additionally, future studies should not solely focus on adverse birth outcomes but also maternal outcomes.
Conclusion
The currently available research supports using maternal MUAC as the most appropriate anthropometric measurement and rapid assessment tool for identifying pregnant women as acutely undernourished and potentially in need of nutritional intervention to prevent adverse birth outcomes. This is particularly noteworthy in resource-limited settings, such as protracted humanitarian settings or emergencies. An advantage of measuring MUAC is that it requires minimal training and is reliable in identifying nutritional status. Initially, there has been no universal absolute cut-off value identified; however, this review supports the specific cut-off threshold for maternal MUAC in this context as <23 cm.
For more information, please contact Sonia Kapil at soniackapil@gmail.com
Editor’s note
The importance of developing guidance to treat maternal undernutrition in humanitarian contexts for both improved birth and maternal outcomes is currently being explored within a Women’s Nutrition Taskforce established within the Global Nutrition Cluster Technical Alliance. The results of this review are being used by the Taskforce to inform the development of operational guidance for women’s nutrition in humanitarian contexts.
References
Adane T & Dachew BA (2018) Low birth weight and associated factors among singleton neonates born at Felege Hiwot referral hospital, North West Ethiopia. African Health Sciences, 18, 4, 1204–1213.
Degno S, Lencha B, Aman R et al. (2021) Adverse birth outcomes and associated factors among mothers who delivered in Bale zone hospitals, Oromia Region, Southeast Ethiopia. The Journal of International Medical Research, 49, 5.
Haque MA, Choudhury N, Farzana FD et al. (2021) Determinants of maternal low mid-upper arm circumference and its association with child nutritional status among poor and very poor households in rural Bangladesh. Maternal & Child Nutrition, 17, 4, e13217.
Kpewou DE, Poirot E, Berger J et al. (2020) Maternal mid-upper arm circumference during pregnancy and linear growth among Cambodian infants during the first months of life. Maternal & Child Nutrition, 16, S2, e12951.
Nyamasege CK, Kimani-Murage EW, Wanjohi M et al. (2019) Determinants of low birth weight in the context of maternal nutrition education in urban informal settlements, Kenya. Journal of Developmental Origins of Health and Disease, 10, 2, 237–245.
Siyoum M & Melese T (2019) Factors associated with low birth weight among babies born at Hawassa University Comprehensive Specialized Hospital, Hawassa, Ethiopia. Italian Journal of Pediatrics, 45, 1, 48.
Sphere Association (2018) The Sphere Handbook: Humanitarian Charter and Minimum Standards in Humanitarian Response (4th ed.). Geneva, Switzerland.
Tesfa D, Tadege M, Digssie A et al. (2020) Intrauterine growth restriction and its associated factors in South Gondar zone hospitals, Northwest Ethiopia. Archives of Public Health, 78, 89.
Vasundhara D, Hemalatha R, Sharma S et al. (2020) Maternal MUAC and fetal outcome in an Indian tertiary care hospital: A prospective observational study. Maternal & Child Nutrition, 16, 2, e12902.
Ververs MT, Antierens A, Sackl A et al. (2013) Which anthropometric indicators identify a pregnant woman as acutely malnourished and predict adverse birth outcomes in the humanitarian context? PLoS Currents, 5.


