Benefits of an integrated stunting prevention programme in Afghanistan
Mona Shaikh Head of Nutrition at World Food Programme (WFP), Afghanistan
Cyprian Ouma Nutrition Evidence Generation Officer at WFP, Afghanistan
Said Shamsul Islam Shams Programme Policy Officer-Nutrition at WFP, Afghanistan
Rogers Wanyama Deputy Head of Nutrition WFP Afghanistan
Professor Sajid Soofi Associate Director, Department of Paediatrics and Child Health, Division of Woman and Child Health, Medical College, Aga Khan University, Pakistan
The authors would like to acknowledge the work of the Public Nutrition Department, Ministry of Public Health, Afghanistan, and the communities present in the intervention and control districts. We thank the WFP, Aga Khan Foundation, Aga Khan Health Services, AKU Academic Projects, and the Centre of Excellence in Women and Child Health, Aga Khan University, Pakistan, for their support.
What we know: Interventions that provide an integrated package of specialised nutritious foods, local diet promotion, and social and behaviour change communication (SBCC) strategies are associated with improvements in key nutrition outcomes during the first 1,000 days.
What this adds: This article reports on the benefits of an 18-month stunting prevention programme providing specialised nutritious foods in combination with SBCC in Badakhshan province, Afghanistan. Results suggest a significant impact on reducing stunting and corresponding improvements in reported infant and young child feeding (IYCF) practices. Despite some limitations to the study, these findings add to the evidence base for promising interventions to address stunting in the challenging context of Afghanistan.
Nutritional supplementation, with or without SBCC, is a proven intervention for preventing malnutrition in many developing countries (Bhutta et al, 2008; Mahumud et al, 2022). However, studies often overlook local factors, which limits their applicability at community level, particularly for a complex context such as Afghanistan.
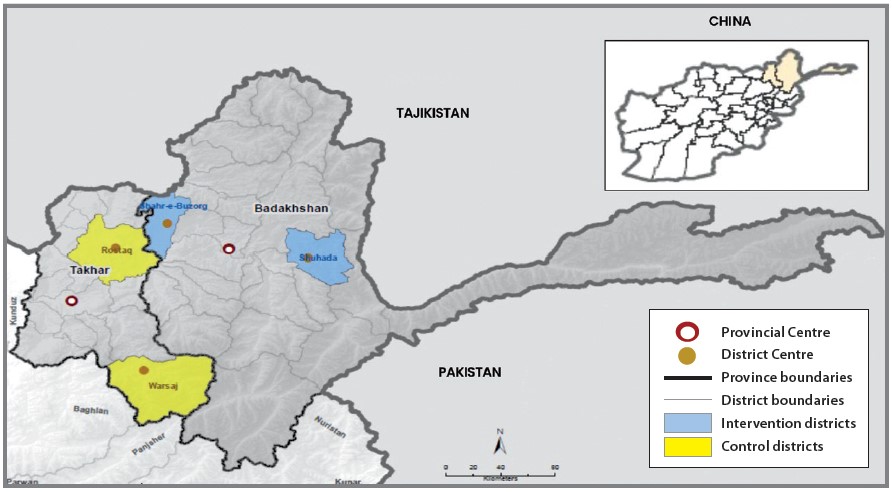
In 2021 and 2022, WFP Afghanistan in collaboration with the Public Nutrition Department of the Ministry of Public Health implemented a stunting prevention programme. Shahri Buzurg and Shuhada districts in Badakhshan province were chosen as locations (Figure 1) for this intervention due to the high stunting prevalence of 58% at the provincial level (Government of Afghanistan & UNICEF, 2014). The programme was implemented through existing health systems, with monthly delivery of interventions supported by Aga Khan Health Services Afghanistan. At the community level, community health workers (CHWs) and mobile health teams were supported by the Aga Khan Foundation.
Figure 1: Intervention and control areas within north-east Afghanistan
Methodology
The intervention package
The interventions were focused on providing specialised nutritious foods to eligible beneficiaries and SBCC messages delivered through existing health systems, mobile health teams, and CHWs. All children aged 6-23 months received a monthly ration of 30 sachets of locally produced lipid-based nutrient supplement-medium quantity (LNS-MQ). Pregnant and breastfeeding women (PBW) received a monthly ration of 7.5kg super cereal (250g per day). This was distributed during the period January 2021 to June 2022. LNS-MQ (or ‘Wawa Mum’) was made with heat-treated oil, seeds, pulses, cereals, milk powder, sugar, vegetable oils, vitamins, and minerals. A 50g daily sachet provided 255 Kcal.
For the SBCC implementation, a cascade training approach was followed, involving an initial training of master trainers followed by training for health facility staff and CHWs. To create awareness in the community and at the household level, female and male support groups were strengthened in the catchment areas of CHWs. Monthly parents’ group meetings were arranged with the assistance of the community support group and health workers, to disseminate SBCC messages related to IYCF practices, child and maternal nutrition, and the use of nutritional supplements. Community mobilisers in the intervention group conducted separate sessions for PBW, mothers-in-law, fathers, and fathers-in-law using educational materials (flip charts) on optimal IYCF practices and maternal and child nutrition. Because of their important role in decision making, male family members were encouraged to participate actively in these sessions.
Study design
A quasi-experimental design was used to evaluate the impact of the integrated intervention package. The primary outcome was stunting prevalence for children aged under two years. Secondary outcomes included child wasting, underweight and anaemia, reported IYCF practices, nutrition status and dietary diversity among PBW, and antenatal care access. Pre- and post-intervention assessments were conducted in both intervention and control districts. The project was implemented for approximately 18 months, with the baseline survey conducted between October and December 2020 and the endline survey between July and August 2022.
Difference-in-difference (DD) estimates were calculated using a generalised linear regression model. This was adjusted for: child gender and age; maternal age, education, and BMI; the presence of a skilled birth attendant; births in a facility; IYCF practices; and household characteristics. Takhar province was selected as the control area (Rustaq and Worsaj districts) as these locations were comparable in accessibility, socioeconomic conditions, geography, and ethnicity at the start of the programme.
Despite similarities, there were significant intra- and inter-district fluctuations in ethnicity at baseline and endline. Other significant socioeconomic changes could be seen with household ownership status, improved water access, household materials, and livestock ownership. Each of these cases was attributed to a combination of seasonal highland and lowland livestock migration and the NATO withdrawal from the country, which occurred mid-programme (2021). These factors are important, as they do make it more difficult to interpret the results since observations could be linked to these underlying population dynamics.
A total of 2,912 children aged under two years and their mothers (1,456 per group per survey) were estimated to provide reasonable precision for baseline and endline surveys. This was based on a 13% relative reduction in the prevalence of stunting in children aged under two years in the intervention vs control group.
All PBW with children aged under two years were eligible to complete the baseline and endline surveys. Eligible participants were identified through two sources. At health facilities, a list of pregnant women who accessed antenatal care services and breastfeeding mothers who accessed postnatal care and childcare services were prepared. At the community level, a list of PBW and children was prepared through CHWs. This included those PBW and children who were not captured at the health facility level. The data collection teams prepared a list of all the PBW with children aged under two years from each health facility and CHW. Households from each village were randomly selected to participate in the survey.
Discussion
Stunting
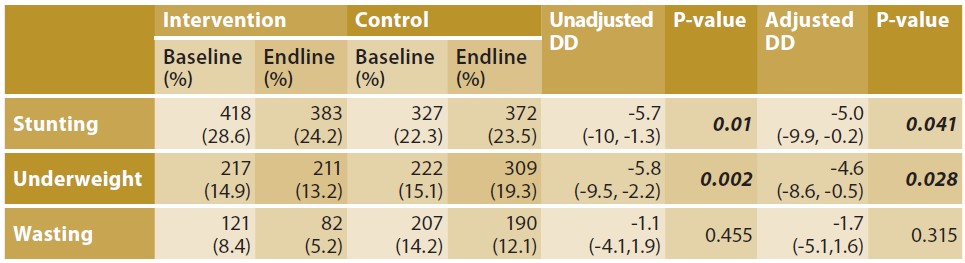
We observed a significant reduction in stunting prevalence (height-for-age <-2 z-scores) among children aged under two years in the intervention group (28.6% baseline; 24.2% endline, p=0.006). In the control group, there was a small increase in stunting prevalence, but this was not statistically significant (22.3% baseline; 23.5% endline). DD estimates indicated a significant reduction in stunting after adjusting for relevant confounders (DD -5.0%; p=0.041) (Table 1). In fact, DD analysis showed that the intervention group saw significant reductions in stunting prevalence both before and after adjustment for common confounders. This is important, as it may indicate that the effect was independent of other factors and that it may be attributed to the intervention with a greater degree of confidence. In line with findings reported from other settings, we found that stunting was more common among boys than girls in both intervention and control groups (Thurstans et al, 2020).
Table 1: Difference-in-difference (DD) among children aged under two years in control and intervention groups
Underweight
Among children aged 6-23 months in the intervention group, the survey found no significant reduction in the prevalence of underweight (weight-for-age <-2 z-scores), which remained relatively stable throughout (14.9% baseline; 13.2% endline). DD estimates indicated a significant reduction in underweight (DD 4.6%; p=0.028). However, this difference was due to the prevalence of underweight increasing in the control group, rather than a reduction in underweight prevalence in the intervention group (Table 1). This suggests that the interventions were possibly protective against the deterioration of underweight in the intervention locations. In the intervention group, improvement in underweight prevalence was statistically significant among girls (14.6% baseline; 10.8% endline, P=0.03). This matches the stunting findings, where girls tended to improve more than boys.
Wasting
Although wasting prevalence in the intervention group reduced significantly (8.4% baseline; 5.2% endline) p=<0.001), the prevalence of wasting also reduced in the control group (14.2% baseline; 12.1% endline) with overall no statistically significant difference in DD (Table 1). The patterns observed for stunting and underweight were comparable to wasting, which was higher among boys at baseline and endline overall.
Other findings
It is notable that the percentage of women seeking antenatal care during pregnancy improved within the intervention group (67.8% baseline; 93.7% endline). However, there was no significant change in the control group (84% baseline; 88.6% endline). This improvement may indicate a possible pathway to stunting reduction.
Over 90% of PBW in the intervention group and 59.7% in the control group received additional messages regarding the intake of five different food groups every day. Nearly all PBW in the intervention group (97.4%) reported receiving the message regarding super cereal, versus 20.3% of PBW in the control group. This suggests some spillover of the SBCC messaging. Compared to the control group, a higher proportion of PBW in the intervention group (97.0% vs 63.3%) reported receiving messages about initiating breastfeeding within the first hour of birth, continued exclusive breastfeeding, and introduction of age-appropriate complementary foods along with breastfeeding. Overall, these results indicate the intervention was effective in increasing the coverage of IYCF messaging.
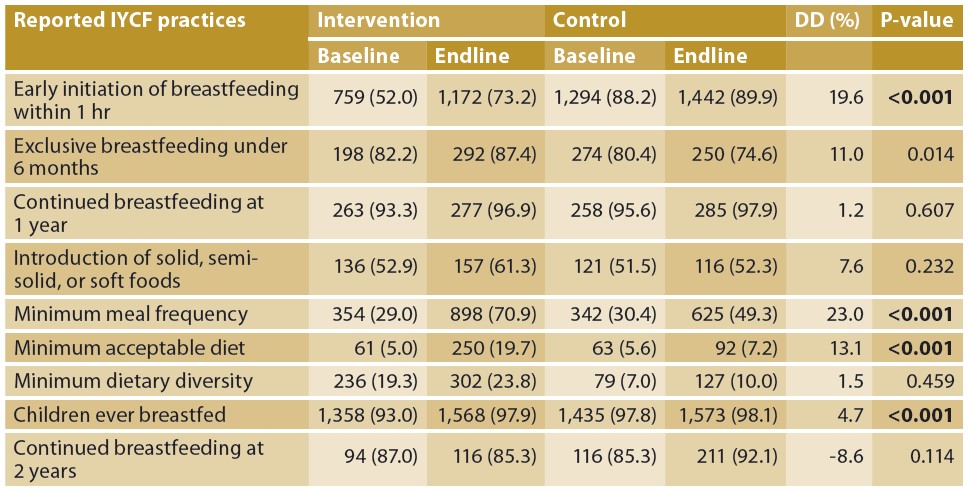
The DD analysis suggests that the SBCC component was effective in improving IYCF practices that are instrumental in the pathway to stunting reduction. Estimates showed significant improvements in early initiation of breastfeeding (within one hour of birth), exclusive breastfeeding aged under six months, minimum meal frequency, minimum acceptable diet, and children ever breastfed (Table 2).
Table 2: Reported IYCF practices in control and intervention groups by difference-in-difference estimates
Strengths and limitations
The large sample size for this study was a major strength. In addition, both baseline and endline survey instruments asked about a wide range of maternal and child health outcomes, some of which were targeted by the intervention and some that were not. Data collection was also completed in the local language, which likely increased inclusivity and may have reduced the risk of information bias. The data was also carefully reviewed to find outliers and unlikely responses. It is notable that data collection occurred between 2020 and 2022 and is therefore now a few years old, although many of the findings remain relevant and key takeaways important.
In addition to the super cereal (provided to PBW) and the lipid-based nutrient supplements (provided to children aged 6-23 months), another intervention (ready-to-use therapeutic food) was delivered simultaneously in both intervention and control districts as a part of national integrated management of acute malnutrition programming. This affected a small percentage of children (6.3%) and PBW (11.9%) in control districts. Although small, these numbers should be considered when interpreting the results.
Parallel interventions reflect the real-world nature of programming. Although they make data interpretation more difficult, they do highlight the importance of a multifaceted, integrated package of interventions that can tackle multiple pathways. It is likely that parallel interventions had some impact on the outcomes measured, although it is difficult to determine the exact degree. However, the findings from this study highlight impressive reductions in stunting, as well as other outcomes, with large effect sizes observed both before and after adjustment.
Lessons learned
Participation in the intervention combining specialised nutritious foods with SBCC over an 18-month period was associated with significant reductions in stunting prevalence among children aged under two years. With stunting being our primary outcome of interest, these results are encouraging. A large effect size was observed, which increases our confidence in these findings.
It is difficult to determine the effect that underlying population changes and migration dynamics had on these results. This, once again, highlights the challenge of conducting such large studies in volatile regions. Despite the limitations, this work is important in providing evidence from a challenging context. The finding that combining special nutritious foods with SBCC in the first 1,000 days may have a significant impact on stunting and underweight has important implications.
Addressing stunting in Afghanistan remains a critical public health concern. Multisectoral approaches that promote community engagement and participation are key to achieving sustained positive outcomes and require an appropriately trained workforce. Increasing the evidence base for how best to deliver SBCC, promote local, healthy diets, and optimise nutrition commodity use in this complex context should be prioritised.
Building on this, WFP, again in partnership with Aga Khan University, is implementing a new community-based stunting reduction programme targeting children under two years and PBW. Integrated interventions will include nutrition assessment, distribution of specialised nutritious food, promotion of local diets through local nutritious seasonal foods, appropriate maternal, infant, and young child feeding practices, and SBCC. In support of further evidence generation, the 18-month programme will incorporate a longitudinal cohort study design, combined with cross-sectional surveys, and a process evaluation. This new study will investigate the impact of duration and modality of the intervention as well as the influence of other contextual factors on the nutrition outcomes of the target groups.
For more information, please contact Mona Shaikh at mona.shaikh@wfp.org
References
Bhutta Z, Ahmed T, Black R et al (2008) What works? Interventions for maternal and child undernutrition and survival. The Lancet, 371, 9610, 417-440
Government of Afghanistan & UNICEF (2014) National nutrition survey Afghanistan. reliefweb.int
Mahumud R, Uprety S, Wali N et al (2022) The effectiveness of interventions on nutrition social behaviour change communication in improving child nutritional status within the first 1000 days: Evidence from a systematic review and meta-analysis. Matern & Child Nutrition, 18, 1, e13286
Thurstans S, Opondo C, Seal A et al (2020) Boys are more likely to be undernourished than girls: A systematic review and meta-analysis of sex differences in undernutrition. BMJ Global Health, 5, e004030
About This Article
Jump to section
Download & Citation
Reference this page
Shaikh M, Ouma C, Shamsul Islam Shams, S, Wanyama R & Soofi S (2025) Benefits of an integrated stunting prevention programme in Afghanistan. Field Exchange issue 75. Emergency Nutrition Network (ENN), Oxford, UK. https://doi.org/10.71744/jz13-jz14


