Opportunities to improve undernutrition and tuberculosis management in paediatric care
Catherine Hewison Intersectional Tuberculosis Platform Tuberculosis Leader, Médecins Sans Frontières (MSF), France
Kerstin Hanson Intersectional Nutrition Platform Leader, MSF, France
Johanna Thomson Intersectional Paediatric Platform Leader, MSF, France
Stijn Deborggraeve Advocacy Advisor Paediatric Tuberculosis, MSF, Belgium
Oluwakemi F. Ogundipe Child Health Advisor, MSF, Belgium
Daniel Martinez Garcia TACTiC Project Leader, MSF, Switzerland
What we know: Tuberculosis (TB) and undernutrition are strongly linked. Undernutrition increases the risk of developing TB and poor outcomes from TB, while TB can both cause and worsen undernutrition. Diagnosis, treatment, and prevention of TB among children can be challenging, particularly in humanitarian and resource-limited contexts.
What this adds: Recently updated World Health Organization (WHO) recommendations offer opportunities to positively impact the management of TB among undernourished children. One of the main additions is the use of a decision tree to be able to diagnose children with TB in humanitarian and resource-limited contexts, even in the absence of conventional diagnostic tools. Improvements in preventative TB treatment for children and food assistance for household contacts of TB patients are other promising developments.
TB is the biggest infectious disease killer globally, causing over 1 million deaths annually. TB is caused by bacteria spread through the air when an infected person coughs or sneezes. It most often affects the lungs (pulmonary TB) but can affect any part of the body (extrapulmonary TB). In 2023, 10.8 million people fell ill with TB worldwide. Of the estimated 1.3 million affected children aged under 15 years old, 45% are never diagnosed. Around 96% of the estimated TB-related deaths are among these children, who have never accessed TB treatment. Most people infected by TB bacteria never develop the disease, but those with a compromised immune system have increased risk. Thus, since adequate nutrition is needed for a strong immune system, poor nutritional status is one of the major TB determinants, with over 1 million cases of TB each year attributed to undernutrition (WHO, 2024a; Dodd et al, 2017).
Undernutrition is not only a factor leading to the development of TB disease after infection but is also a significant consequence of TB. Young children are inherently more vulnerable as their immune systems are still developing, are at more risk of undernutrition, and can become ill more easily. When they fall ill they also become more severely unwell and more frequently die from illness.
Despite the large global burden of TB, there has been chronic under-investment in research and development for tools dedicated specifically to children and humanitarian and resource-limited settings. In particular, lack of prioritisation has resulted in inadequate tools for early detection, timely treatment, and effective prevention of TB in this vulnerable population.
Recent and upcoming recommendations from the WHO present an opportunity to address some of the challenges and improve upon the status quo. These are discussed further below. New recommendations for nutrition and TB are expected to be released in 2025. In addition, the 2023 WHO guideline on the prevention and management of wasting and nutritional oedema includes recommendations for children with co-morbidities such as TB (WHO, 2023).
As a medical humanitarian organisation, MSF, also known as Doctors without Borders, frequently encounters children with TB and undernutrition, and the associated challenges. This inspired MSF to develop the TACTiC (Test Avoid Cure TB in Children) project, a multi-country project to improve the management of TB in MSF projects and beyond. The project has three pillars: 1) implementation of the various WHO recommendations; 2) operational research on the effectiveness, feasibility, and acceptability of the recommendations; and 3) advocacy for the implementation of currently available tools, as well as for more research and development into better adapted tools for the management of TB in children.
Drawing on our experience within the TACTiC project, in this article we describe challenges in the management of TB in children with undernutrition and steps toward improvement.
Challenges in tackling TB among children affected by undernutrition
Difficulties in diagnosis
Weight loss or failure to gain weight are classic symptoms of TB. One would therefore expect that it would be simple to screen all children with undernutrition to rule out TB as a cause. Diagnosing TB in children can, however, be very challenging. A contributing factor is the lack of tests adapted to children. Children develop TB disease with a very low number of Mycobacterium tuberculosis (M.tb), the bacteria causing TB. Current microbial tests are not sensitive enough to pick up the low number of M.tb that is causing illness. Preliminary results from MSF studies show that less than 10% of children diagnosed with TB have a positive test. Furthermore, current tests usually rely on sputum (spit) samples. Sputum is difficult to collect from children, especially the youngest ones, as it requires coughing up sputum from their lungs, following instructions that children might struggle with.
Children are also more frequently affected by extra-pulmonary TB, such as bone TB or TB meningitis. Collecting samples from the affected area for testing is even more challenging. Furthermore, symptoms resemble those of many other diseases, adding to the diagnostic challenges. Clinicians must therefore rely primarily on clinical observations and a high-level awareness of TB as a potential diagnosis, complemented by microbial testing and radiology, to decide on treatment.
Overcoming these challenges is particularly urgent for children that are undernourished or younger than two years old who, along with children living with HIV, are at highest risk of death from TB and where delays in diagnosis are often deadly (Vonasek et al, 2022).
Lack of integrated programming
At a programmatic level, the vertical nature (addressing specific diseases in standalone programmes) of TB and nutrition programmes pose a barrier to an integrated approach (Patel & Detjen, 2017). These programmes often run in parallel, with independent sources of funding and coordination, as well as disease-specific objectives and priorities. Most children affected by undernutrition and TB present for care through nutrition programmes, which have little capacity to screen, test, or treat TB cases. Access to space, medicine, appropriately trained staff, and infrastructure such as X-ray and laboratory capacity to conduct bacteriological testing for TB are particularly constrained in humanitarian and resource-limited contexts. In crises, emergency interventions around access to food, water, shelter, and outbreak management are prioritised, leaving little capacity to identify and treat TB among children with undernutrition.
Stigma
Stigma surrounding TB and misconceptions about undernutrition can also result in inadequate recognition of symptoms, as well as delays in diagnosis and treatment of TB in this vulnerable group.
Steps for improving the management of children with undernutrition and TB
Informed by new evidence, in 2022 WHO issued new recommendations that offer an opportunity to make a real positive impact on TB management amongst children suffering from undernutrition (WHO, 2022a). Several recommendations stand out in their potential to revolutionise the approach to care for this vulnerable demographic.
Use of treatment decision algorithms
Firstly, WHO recommends the use of treatment decision algorithms (Figure 1) to facilitate clinical decision making and rapid initiation of TB treatment for children aged under 10 years with pulmonary TB. There are two algorithms, one for use where chest X-ray is available and one where it is not (Figure 1). A key feature of the algorithms is the fast-tracking of treatment initiation for children with highest risk of mortality, including those presenting with severe wasting as well as children aged under two years and those living with HIV. The algorithms include a scoring system that uses clinical signs and symptoms, and X-ray findings if available, to decide on treatment initiation. Although laboratory testing for TB is encouraged, even if testing is unavailable or a negative result is obtained this does not hinder starting treatment based on clinical symptoms alone. The algorithms are also designed to encourage repeated assessment when indicated. WHO made an interim recommendation on the use of these algorithms (WHO, 2022b). MSF is among the organisations answering the WHO call for operational research documenting their use in real-life settings.
Figure 1. WHO’s algorithm B* (page 74, WHO 2022b) for children <10 years of age for settings without X-ray.
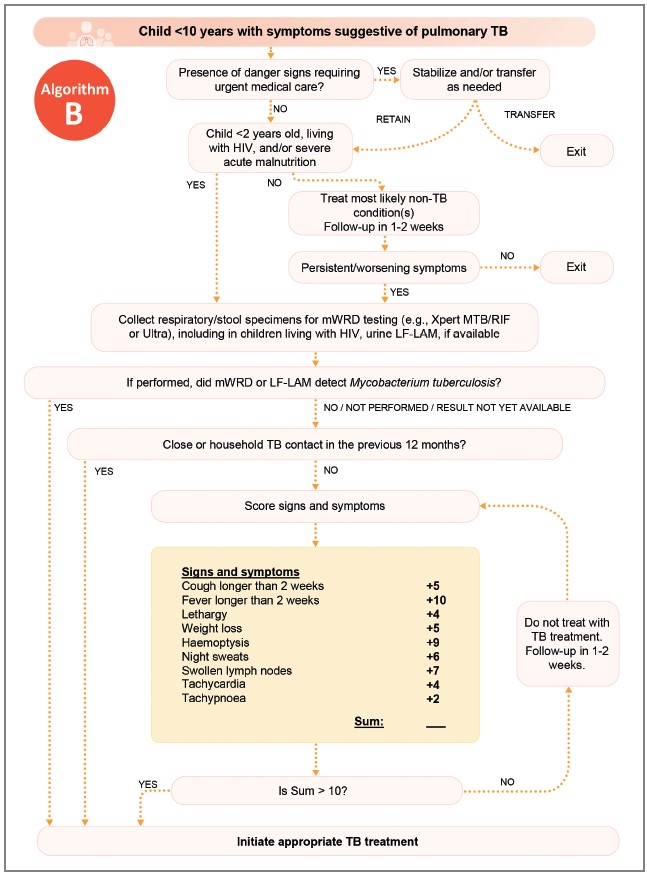
*Algorithm A (not depicted) is for settings with chest X-ray. ‘mWRD’ and ‘LF-LAM’ are different laboratory tests.
Data from MSF projects implementing the WHO-recommended treatment decision algorithms in therapeutic feeding programmes have shown a 1.5- to five-fold increase in the number of children with severe wasting diagnosed with TB. Preliminary results from an ongoing MSF study on implementation of the algorithms in five African countries show that up to 80% of children diagnosed with TB are diagnosed via the algorithm’s clinical score rather than laboratory test results. This applies whether using the algorithm with or without chest X-ray.
These results emphasise the importance of clinical decision making when deciding whether to treat children for TB. They also illustrate how the algorithms facilitate the decision to treat TB in undernourished children, even without access to X-ray or laboratory testing, or in the case of negative results (which can be expected in children with wasting).
Reducing the duration of TB preventive treatment
WHO recommends a short three-month treatment to prevent the development of TB disease among children who are likely to have been infected by TB by living in the same household as a person affected by TB disease. This preventive treatment can reduce the number of children developing TB disease. The short duration and the availability of new child-appropriate drug formulations for all ages should have an important impact on their scale-up (WHO, 2024b).
Food assistance for household contacts of TB
In 2024, WHO convened a Guideline Development Group to review available data on TB and undernutrition. The updated version of WHO’s 2013 recommendations on TB and nutrition (WHO, 2013) is expected in early 2025. Data from the RATIONS trial in India found that food assistance to all household contacts of a TB case reduced the number of people in the household who developed TB disease (Bhargava et al, 2023).
Integrated protocols, guidance, and decision making
To effectively manage paediatric TB and undernutrition, collaboration between nutrition and TB services is essential. This can be facilitated by the harmonisation of guidance documents, in particular the inclusion of TB treatment decision algorithms in national guidelines for the management of wasting. Clear guidelines that dictate the appropriate contexts and circumstances for utilising treatment decision algorithms will ensure a streamlined diagnostic process rather than additional workload. This includes creating pre-screening questionnaires and decision trees tailored for busy healthcare environments, enabling healthcare workers to more efficiently identify at-risk children and refer or initiate TB treatment when indicated.
In the long term, integration of TB and nutrition services into national health programmes will ensure that management of both TB and undernutrition in children is aligned with broader health goals. Advocacy aimed at making TB a priority within national health agendas is critical for mobilising the resources and attention necessary for comprehensive care.
Improving capacity of healthcare workers
Increasing the clinical capacity of healthcare workers in general paediatric care as well as the clinical overlap between TB and undernutrition is crucial for improving diagnostic accuracy. Capacity-building initiatives can empower frontline health workers to navigate the various illnesses that affect vulnerable young children and to acquire the competencies to recognise the often-subtle signs of TB in malnourished children.
Community engagement and awareness
Community engagement plays a vital role in reshaping perceptions around TB and undernutrition, and enhancing TB awareness within communities can reduce stigma and promote early healthcare-seeking behaviour among families. Hearing from communities on how to best tailor TB services to their needs can also contribute to improved treatment experiences and results.
Utilising peer support groups and community health workers can facilitate education and support for families grappling with the compounded challenges of TB and undernutrition. Empowering families with knowledge about the risks and symptoms of TB can lead to timely interventions and increased adherence to treatment, including preventive treatment.
Improved monitoring and evaluation
Implementing effective strategies requires ongoing monitoring and evaluation to assess the impact of integrated care interventions on health and nutrition outcomes for children with TB and undernutrition. Continuous feedback loops integrating children and their families, healthcare workers, and policymakers will enable all stakeholders to refine their approaches based on real-time data, enhancing both programme efficacy and responsive resource allocation.
Data collection on paediatric TB cases in undernourished populations should be prioritised, allowing for a better understanding of the epidemiological trends and disease burden. By leveraging technology such as digital health tools, stakeholders can streamline reporting processes and enhance data accessibility, promoting a culture of transparency and accountability.
Conclusions
TB affects children with undernutrition disproportionally, especially children with severe wasting where the risk of death is high. The best tools currently at our disposal to detect and manage TB among undernourished children are the WHO treatment decision algorithms combined with the vigilance and skills of healthcare workers. Investment in research and development is needed for the elaboration of better diagnostic tools, adapted to the needs of children with TB. Implementation of household food assistance and providing preventive TB treatment to children who are household contacts of TB cases have the potential to substantially reduce the incidence of TB disease in this vulnerable group.
Integration of nutrition and TB services into national health frameworks is key. As is engaging communities and addressing supply, logistical, and human resource challenges in ways that could increase the number of undernourished children diagnosed and treated for TB. This could improve timely treatment and so ultimately reduce mortality in this vulnerable group. Nowhere is this more needed than in humanitarian and resource-limited contexts.
For more information, please contact Catherine Hewison at cathy.hewison@paris.msf.org
References
Bhargava A, Bhargava M, Meher A et al (2023) Nutritional support for adult patients with microbiologically confirmed pulmonary tuberculosis: Outcomes in a programmatic cohort nested within the RATIONS trial in Jharkhand, India. The Lancet Global Health, 11(9), e1402–e1411
Dodd PJ, Yuen CM, Sismanidis C et al. (2017) The global burden of tuberculosis mortality in children: A mathematical modelling study. The Lancet Global Health, 5(9), e898–e906
Patel LN & Detjen AK (2017) Integration of childhood TB into guidelines for the management of acute malnutrition in high burden countries. Public Health Action, 7(2), 110–115
Vonasek BJ, Radtke KK, Vaz P et al (2022) Tuberculosis in children with severe acute malnutrition. In Expert Review of Respiratory Medicine (Vol. 16, Issue 3, pp. 273–284). Taylor and Francis
WHO (2013) Guideline: Nutritional care and support for patients with tuberculosis. who.int
WHO (2022a) WHO consolidated guidelines on tuberculosis. Module 5: Management of tuberculosis in children and adolescents. iris.who.int
WHO (2022b) WHO operational handbook on tuberculosis. Module 5: Management of tuberculosis in children and adolescents. iris.who.int
WHO (2023) WHO guideline on the prevention and management of wasting and nutritional oedema (acute malnutrition) in infants and children under 5 years. who.int
WHO (2024a) Global Tuberculosis Report 2024. who.int
WHO (2024b) WHO consolidated guidelines on tuberculosis: Module 1: Prevention: Tuberculosis preventive treatment. iris.who.int
About This Article
Download & Citation
Reference this page
Hewison C, Hanson K, Thomson J, Deborggraeve S, Ogundipe OF & Martinez Garcia D (2025) Opportunities to improve undernutrition and tuberculosis management in paediatric care. Field Exchange issue 75. Emergency Nutrition Network (ENN), Oxford, UK. https://doi.org/10.71744/tn29-ej38


