Treatment of severe acute malnutrition through the Integrated Child Development Scheme in Jharkand State, India
By Grana Pu Selvi and Colleen Emary
 |
Click here to listen to an interview with the authors on the ENN podcast channel |
Grana Pu Selvi has postgraduate qualifications in food and nutrition and international public health. She has been working with World Vision India for the past seven years leading a country-wide maternal, newborn, child health and nutrition intervention.
Colleen Emary is a public health nutritionist with 17 years’ experience in international public health nutrition. She currently works as a health and nutrition technical advisor with World Vision International, based in Canada.
The authors would like to thank the State Nutrition Mission, Jharkhand for giving the opportunity and ongoing support to implement this programme, World Vision Hong Kong for its financial support and World Vision India for its leadership and support to pilot this programme. The authors would also like to express their appreciation for the dedicated work of Sudhakar Subburayan of World Vision India, who has been instrumental in piloting the community-based management of acute malnutrition (CMAM) project in coordination with the respective departments in Bokaro district.
Location: Jharkhand State, India
What we know: The prevalence of acute malnutrition in India is high; community-based management of acute malnutrition (CMAM) is not widely implemented.
What this article adds: A flagship pilot outpatient severe acute malnutrition (SAM) treatment programme was implemented through the Integrated Child Development Scheme in Bokaro district by World Vison India in collaboration with Jharkhand State Nutrition Mission. Fifty-one outpatient therapeutic programme sites were established at existing anganwadi centres; existing staff were trained and 40 volunteers recruited. Caseload was identified through household screening based on mid-upper arm circumference <11.5 cm. Complicated cases were referred to existing inpatient services. In 2017 the cure rate was 61%, the death rate was 0% and the defaulter rate was 39%. Factors contributing to the high defaulter rate included poor tolerance of ready-to-use therapeutic food, migration, festivals and duration of minimum stay (eight weeks). Areas for improvement include stronger community mobilisation, better integration of medical care in outpatient care, coordination with other SAM treatment services, and harmonised inpatient/outpatient protocols and systems. An external partner remains necessary to provide overall coordination, capacity-building, technical oversight and monitoring/evaluation support.
Background
The Indian State of Jharkhand recently joined the Scaling Up Nutrition (SUN) Movement; one of three in India to do so. India’s national survey data (for 2015-2016) reported 21% prevalence of global acute malnutrition (GAM) (weight-for-height z-score (WHZ) <-2 SD), with 29% GAM and 11.4% severe acute malnutrition (SAM) reported in the State. A baseline survey conducted in March 2016 of World Vision (WV) India programming areas in the Bokaro district of Jharkhand reported 28% GAM (WHZ<-2SD) in children aged 6-59 months.
At the request of the Jharkhand State Nutrition Mission, WV India commenced a pilot outpatient SAM treatment programme (outpatient therapeutic programme (OTP) through the Integrated Child Development Scheme (ICDS) in Bokaro district, the first of its kind in Jharkhand. The ICDS in India is the world’s largest integrated early childhood programme, with over 40,000 centres nationwide1. The programme offers health, nutrition and hygiene education to mothers; informal pre-school education to children aged three to six years; supplementary feeding for all children and pregnant and lactating women (PLW); growth monitoring and promotion; and links to primary healthcare services such as immunisation and vitamin A supplements. These services are provided at anganwadi centres (AWCs); each run by one anganwadi worker (AWW) and one helper. Given the decentralised structure of the ICDS and the proximity of AWCs to the community, this has the potential to be an ideal platform for community-based management of acute malnutrition (CMAM).
The implementation approach in this context used the existing ICDS structure, setting up OTP sites for uncomplicated SAM cases at selected AWCs. Cases of SAM with complications were referred to inpatient facilities at government-run Malnutrition Treatment Centres (MTCs). Within Bokaro, one MTC centre covers three blocks. The pilot project targeted two blocks within Bokaro district; initially Chandankiyari and later expansion to Chas (population 230,238 and 813,402 respectively, as per 2011 census). The purpose of the pilot was to explore the feasibility of using the ICDS system to provide outpatient SAM treatment and documenting lessons learned to inform future policy and programming. The pilot ran from January to September 2017. A post-project evaluation was conducted in September 2017.
This article describes the process of piloting CMAM within the ICDS system, along with the main findings of the project evaluation.

Preparatory phase
A memorandum of understanding (MoU) was signed between WV India and the Jharkhand State Nutrition Mission, outlining roles and responsibilities for the project at state level. The responsibilities of WV India included overall coordination of the procurement of ready-to-use therapeutic food (RUTF) and technical support, while the State Nutrition Mission provided technical advice, periodic review of data and ongoing technical guidance to improve programme quality. In the absence of state-level guidelines for outpatient management of acute malnutrition, WV India drafted operational guidelines, based on international protocols, contextualised for the ICDS implementation environment. This document served as an important technical reference for the project, particularly for WV India.
Local negotiations were undertaken at Bokaro District level to ensure that the necessary support was in place for the pilot, including the provision of equipment, local stakeholder engagement, regular review meetings, and capacity-building. The District Collector, District Social Welfare Officer and Child Development Programme Officer were the key stakeholders engaged to create the necessary enabling environment. There are 384 AWCs in Chandankiyari and 597 in Chas blocks, although not all are operational. An AWC facility assessment checklist was developed to identify potential sites for OTP services. Assessment criteria included structural integrity of the building, size of space, available staffing and equipment.
While MUAC screening had been rolled out in the district through ICDS as part of routine growth monitoring, it was not well implemented. Rather than using existing ICDS growth monitoring records, which were considered incomplete, the local government requested an exhaustive house-to-house MUAC screening of children aged 6 to 59 months prior to OTP start-up. Two hundred and seventeen SAM cases were identified (see Table 1 for screening data).
Table 1: MUAC screening in Chandankiyari and Chas blocks
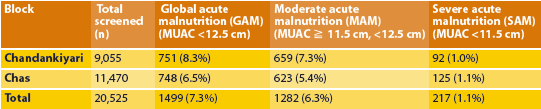
Using the findings of the facility assessment along with MUAC screening results, AWCs were selected as OTP sites that were situated close to families with SAM children and that had the necessary capacity. OTP sites were launched in April 2017, beginning with 14 and increasing to 51 in a progressive manner as SAM cases were identified through house-to-house screening. As Chandankiyari block was the primary focus for the project, OTPs were launched in this block first, followed by Chas.
Training on outpatient management of SAM was provided jointly by the State Nutrition Mission and WV India health and nutrition staff to AWWs, Auxillary Nurse Midwives (ANMs) and Accredited Social Health Activist (ASHA) workers. Across the two blocks, 460 AWWs, 29 ANMs and 80 ASHA workers were oriented on CMAM, with in depth training provided to 40 ANMs and AWWs. Training materials and reference tools (wall posters) were developed for AWWs and ANMs to assist with protocol adherence. In addition, 1,900 AWWs were trained on MUAC measurement and provided with MUAC tapes at district level. Mechanisms were established for management of stock, routine monitoring and supervision through the ICDS system.
As the intent of the pilot was to implement OTP through the ICDS system, existing staff members were used (e.g. AWWs and the ICDS supervisory structure). WV India provided a dedicated CMAM coordinator for the pilot in addition to a network of 40 volunteers supporting nutritional screening, referral and monitoring activities.
Implementation phase
Children aged 6-59 months with a MUAC of <11.5 cm and good appetite were eligible for admission to the AWC OTP. A MUAC-only admission criterion was used, given its stronger association with mortality than WHZ and as it was considered to be most feasible in the context, given the skill level of AWWs. Children with poor appetite or other signs of medical complications were referred to the MTC for inpatient care. Amoxicillin was provided upon admission. Children returned for weekly follow-up sessions. Children had a minimum eight-week stay in the programme and were discharged after eight weeks if their MUAC was >11.5 cm 2. Children who did not reach the discharge criteria by eight weeks were referred to the MTC for further investigation and treatment. Upon discharge children were enrolled in AWC services which included a supplementary feeding programme (SFP).
The MTC provided care for complicated cases as per the government protocol, which is a standard of two weeks of inpatient care, irrespective of whether the child was referred from a community where outpatient treatment for SAM was available. It was not possible within the scope of this pilot to modify MTC protocols and this needlessly extended the inpatient stay of some children, who could have continued their treatment on an outpatient basis once their initial complications had stabilised. During the pilot project, admission rates to the MTC increased by 15% over the same period from the previous year. This was possibly due to increased identification and referral of SAM cases.
Pilot achievements
Fifty-one OTP sites were established at existing AWCs within walking distance (between five and 20 minutes from home), admitting 158 SAM cases over the October to April 2017 period (See Table 2 for treatment outcomes). More girls were enrolled for treatment (63%; n=100) than boys (37%; n=58). Thirty-four cases, representing 21% of admitted children, were referred to MTC from the OTP sites. This level of referral for inpatient care is higher than normally expected and is likely due to an outbreak of chicken pox and measles during the programme period; many children developed fever and lack of appetite as a consequence. It was discovered that routine measles immunisation had not occurred in that community in the last three years. In response, the Department of Health (DoH) was notified and an immunisation campaign was launched in the affected communities. Although 34 children were referred from the OTP to the MTC, only 13 children returned from the MTC to continue treatment in the OTP, with the remaining lost to follow-up. Referral mechanisms were ad hoc, with MTC staff unaware of where OTP AWC sites were located and therefore unable to provide this information to families upon discharge. Referrals relied upon WV India facilitating follow-up and transportation for the families.
Seventy-two children (61%) were discharged as cured from the OTP, meaning that they attained a MUAC of > 11.5 cm with a minimum eight -week stay in the programme. This is below the Sphere Standard of 75%, undoubtedly affected by the high default rate (39%). Reasons for high defaulting were explored through focus group discussions and key informant interviews. The main reasons reported were: poor tolerance of RUTF (loose stools, vomiting), migration for work and attendance at local festivals. The minimum eight-week stay was also noted as a possible reason for high defaulting. A review of defaulting cases found that some children defaulted after five to seven weeks in the programme with a MUAC > 11. 5 m, suggesting that once a child was visibly better the caregiver did not feel it was important to return for the final weeks.
Table 2: Treatment outcomes
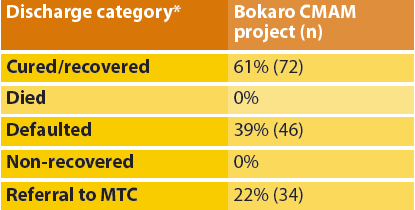
* Definitions for discharges: Cured – child reached discharge criteria (for this project, MUAC > 11.5 cm and minimum eight week stay in OTP); Died – child died while enrolled in OTP; Defaulted – child was absent for three consecutive OTP sessions; Non-recovered – child did not reach discharge criteria after 16 weeks in OTP.
Lessons learned
The project was viewed as appropriate by local stakeholders and in line with local needs. Malnutrition was identified as a significant problem, with the barriers to accessing treatment through MTC acknowledged by all stakeholders. The use of the ICDS as a platform for OTP was viewed as appropriate as it is the most decentralised formal government system, thereby giving the community good access to the programme. Active participation of stakeholders was initially slow at the onset of the project; however, with state and local government leadership, local stakeholders began to value the service provide and fulfilled their respective responsibilities.
The project substantially increased access to SAM treatment, with OTP centres established within walking distance of families affected by SAM. Caregivers reported close proximity of treatment, shortened time required for weekly visits and visible improvements in the health of their children as motivators to attend OTP. In general, the use of RUTF was acceptable to caregivers, although there were some reports of diarrhea and vomiting after consumption.
Local capacity was built within the anganwadi system to manage acute malnutrition. AWCs were open regularly, were staffed and had the necessary supplies. It was perceived that inclusion of the OTP within the AWC improved the overall function of the system. While AWWs reported the feasibility of incorporating SAM treatment into their routine activities, simplified protocols and job aids are needed to match the skill level of AWWs.
While AWWs assumed the primary role for screening and provision of care, medical inputs for routine medication administration and clinical care were to be provided through the health system (ANMs). However, ANMs were not available to provide service on a consistent basis throughout the project. Extensive efforts were made by WV India (e.g. transport, ongoing negotiation with district health authorities) to strengthen this component of the project, however, it remained weak. A tripartite agreement between State Nutrition Mission, Health Department and WV India would help to create the necessary enabling environment to support implementation.
A major area of weakness in project design related to community mobilisation assessment and planning. While there were some activities to sensitise the broader community to the project, most effort was directed at the primary caregiver, usually the mother, with respect to treatment and care of her malnourished child. The important role of other household members (such as father, mother/mother-in-law) in child caring and feeding was not considered and these groups were not directly included in the education and mobilisation activities. In some cases, this made it difficult for the caregiver to provide home treatment of SAM for her child as directed. Future projects should take into consideration these important cultural roles. The lack of effective community outreach undoubtedly contributed to the high defaulter rate and slow recovery rate for some children. Community discussions were needed to share progress of the project with beneficiaries and to address concerns which impacted attendance and acceptance of outpatient treatment for SAM.
In addition, there is an ongoing broader discussion about where CMAM services are best located in Jharkhand. One opportunity is to provide services at sub-centre level (periphery health posts managed by the Health Department), as is currently being done by Médecins Sans Frontières (MSF) in some locations. However, this will reduce accessibility of services as longer travel time is required to reach the sub-centres, which serve a population of 5,000 people. This will need to be resolved to ensure the future sustainability of the treatment services for acute malnutrition.
Recommendations
While the pilot in Bokaro district was the first attempt to use the ICDS as a platform for acute malnutrition treatment services, other actors (MSF, Save the Children and UNICEF) are providing outpatient SAM treatment in Jharkhand through the Department of Health (DoH). Prior to the implementation of this pilot, a consultation with other actors in Jharkhand State to harmonise clinical protocols would have been helpful. It would also have been useful to set up this pilot as an operational research project, which would have allowed for more in-depth analysis of individual child-level data. This required additional resources which were not available at the time.
Rates of GAM and SAM identified through MUAC screening were found to be much lower than previous surveys in Jharkhand State that were based on WHZ. It has been hypothesised that body shape is influencing WHZ (Myatt, 2017), which may partially explain this, but more research is needed on this subject for the India subcontinent. It would also be valuable to monitor children who do not meet the MUAC admission criteria but have a WHZ <-3 SD or WAZ <-3 SD to contribute to the evidence base on the risks of excluding these children.
Harmonisation of MTC and OTP protocols should be undertaken in Jharkhand so that inpatient and outpatient care can be provided in a coordinated manner, rather than as two separate interventions.
In conclusion, the pilot demonstrated that it is feasible to implement outpatient treatment for SAM through the ICDS system. The decentralised structure of the AWCs provide highly accessible service for communities and the AWWs report it is feasible to include outpatient management of SAM within their existing role. However, the current ICDS system cannot deliver OTP services without external support for capacity-strengthening.
An external partner3 is needed to provide overall coordination, capacity-building, technical oversight and monitoring/evaluation support. In addition, a tripartite agreement between State Nutrition Mission (Women and Child Development Department), DoH and external partner is required to ensure clinical/medical care is available at OTPs. If outpatient care for SAM is endorsed by the State and an enabling environment is created for implementation, local capacity can be developed with a view to providing outpatient treatment for SAM as part of routine government services.
For more information, contact Grana Pu Selvi.
Endnotes
1See www.unicef.org/earlychildhood/files/india_icds.pdf
2In the absence of national or state protocols, discharge criteria of minimum eight week stay and MUAC > 11.5cm was used for this pilot, as this criteria had been used in other states in India. Recently, there has a been consensus among the State Nutrition Mission and implementing partners in Jharkand to adopt the WHO-recommended discharge criteria of > 12.5 cm with no oedema for the last two weeks. World Vision has since adopted these criteria.
3World Vision India in the case of this project
References
M Myatt, personal communication, September 27, 2017.


