Supporting healthy growth in infants in low-resource settings in Mumbai, India
By Rupal Dalal, Shruthi Iyer, Marian Abraham and Lahari Yaddanapudi
Rupal Dalal MD FAAP IBCLC is a Founding Medical Director of the Foundation for Mother and Child Health (FMCH), Adjunct Associate Professor at the Centre for Technology Alternatives for Rural Areas (CTARA) and a Project Leader at Health Spoken Tutorial at the India Institute of Technology (IIT), Bombay. She has 14 years’ experience of working in urban slums and rural and tribal areas of India on prevention of malnutrition.
Shruthi Iyer BE is Chief Executive Officer of FMCH. She has 10 years’ experience of working in the development sector with organisations such as Mentor Me India, Hippocampus, Teach for Bangladesh, Masoom and Sukhibhava, working across multiple sectors. She is a Teach for India and Acumen Fellow.
Marian Abraham M.Phil is an Assistant Project Manager at CTARA, IIT, Bombay.
Lahari Yaddanapudi M.Tech has a Masters in Technology and Development from CTARA, IIT, Bombay and is currently an IITB-CTARA Nutrition Fellow.
The authors would like to acknowledge FMCH for providing the opportunity to write about the work of the organisation and share data. Special thanks to Dottie Wagle, who has been at the forefront of the project as chairperson of FMCH for the last 10 years, and who has helped thousands of underprivileged children in Mumbai. The authors would also like to acknowledge District Health Officer Dr Manish Fancy for carrying out the training of medical officers and other field functionaries using Health Spoken Tutorial and sharing their baby’s weight-gain data post-training, and Professor Kannan Moudgalya from Spoken Tutorial Project, IIT B, for providing the platform for the capacity building of healthcare workers through online videos in multiple languages.
Background
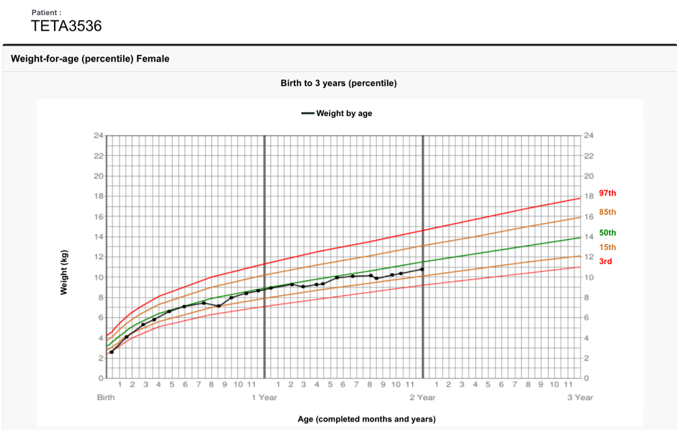
Despite significant reductions over the years, India still has high rates of undernutrition among children under five years of age, 38.4% of whom are stunted, 21.0% wasted and 35.8% underweight (IIPS, 2016a). In addition, an estimated 18.2% of infants are born with a low birth weight (LBW) (IIPS 2016b). Figure 1 demonstrates that, while the prevalence of stunting and underweight increase with age in India, peaking in later infancy and young childhood, the prevalence of wasting is highest between birth and two months of age (IIPS, 2016b). This highlights the in-utero origins of infant undernutrition in this context and the critical importance of interventions to support maternal nutrition in pregnancy and to avert growth faltering and aid catch-up growth in infancy.
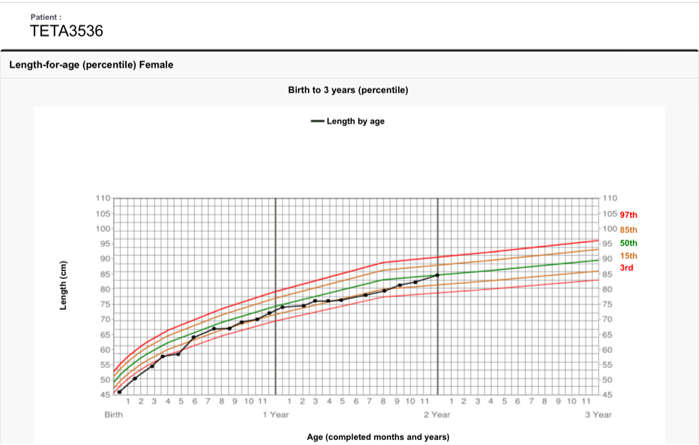
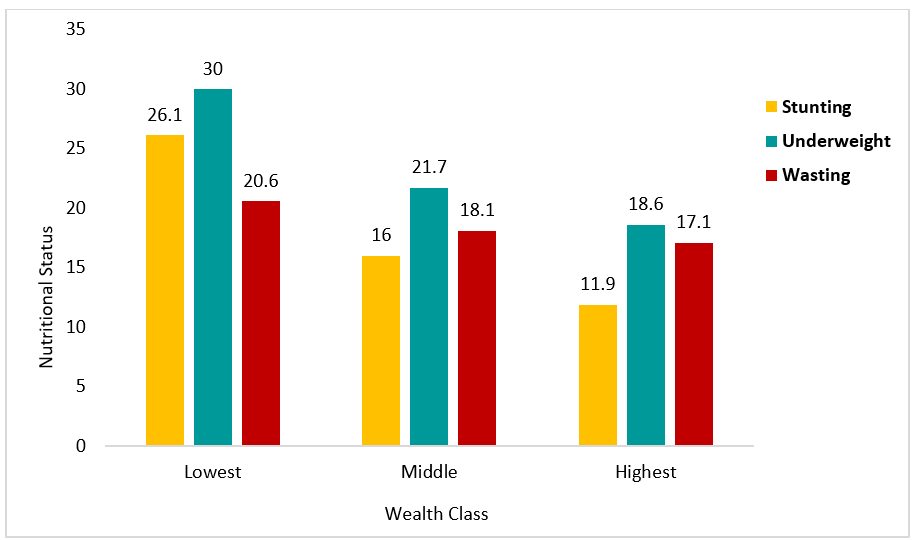
Mumbai is the capital city of the state of Maharashtra on the west coast of India and is the largest, most densely populated city in the country. Analysis of the nutritional status of infants by household wealth in Mumbai shows a strong correlation between undernutrition and low socioeconomic status (poverty); particularly for underweight and stunting (Figure 2). There is also a very high prevalence of LBW among the poorest households in Mumbai (Figure 3), which demonstrates the in-utero origins of undernutrition in this population and the need to focus on optimal nutrition in pregnancy in this vulnerable group.
Figure 1. Nutritional status by age (months) - National Family Health Survey (NFHS-4) 2015-16
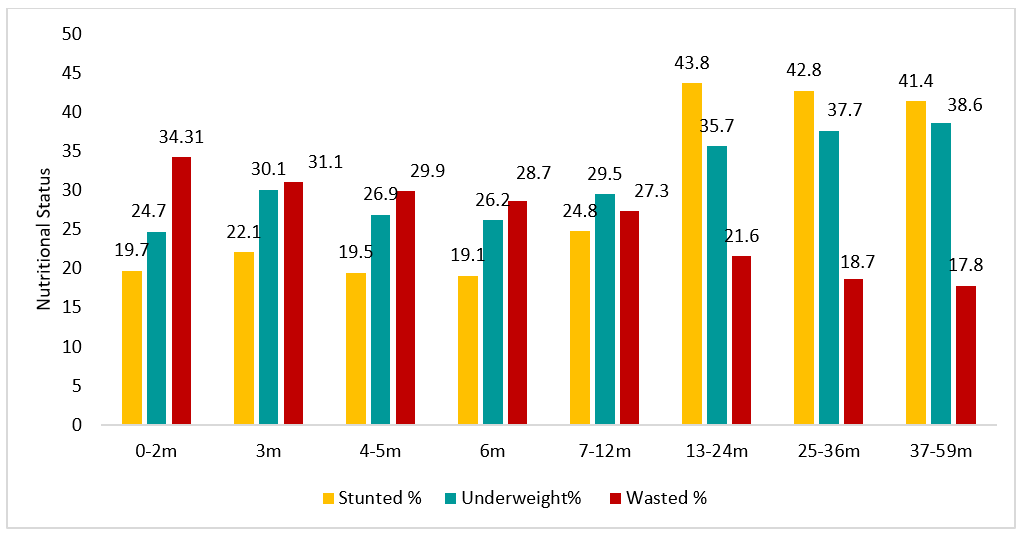
Figure 2. Nutritional status by wealth in Mumbai
Foundation for Mother and Child Health (FMCH) 1,000-days initiative
FMCH is a grassroots organisation founded in 2006 to improve the access of vulnerable communities in the Dhobi Ghat area of Mumbai to health and nutrition interventions. Dhobi Ghat is a low-income area with an estimated population of 50,000, characterised by informal community shanties (‘slums’). As part of its pre-school education programme, FMCH initiated monthly nutrition and health monitoring and catch-up on missed vaccinations for attending children and their younger siblings, as well as nutrition counselling and cooking demonstrations for caregivers. Over time, health and nutrition programming was refocused on the first 1,000 days plus one more year (up to the child’s third birthday), rather than all children under six years of age, as this is the period with most potential to avert growth faltering and reverse the early impacts of undernutrition on stunting in the context of limited programme resources. In response, a set of key activities, displayed in Figure 4 and described below, were implemented in the areas of Ganesh Nagar, Ramdev Nagar and Sukhawani.
Figure 4: Key activities undertaken at Ganesh Nagar, Ramdev Nagar and Sukhawani by FMCH

Newborns and children under three years of age were brought by their mothers/caregivers to the clinics (monthly if weight gain was good and more frequently if not) for mothers/caregivers to receive one-to-one counselling with trained health workers, including field officers, social workers, nurses, nutritionists and a doctor. At each visit, infants and caregivers were supported with:
Growth monitoring: Two trained field officers took weight and length/height measurements of infants using calibrated machines (discrepancies were checked by a third officer). Measurements were entered into a customised, cloud-based software program to generate World Health Organization (WHO) z-scores and automatically plot percentile weight-for-age, length-for-age and weight-for-height charts, and results were shared with the mother/caregiver. If a child was identified with medical complications or developmental delay, they were referred for management at the closest nutrition rehabilitation centre or paediatric hospital as appropriate.
Breastfeeding support and counselling for mothers of infants and young children: Breastfeeding mothers and their infants were assessed using digitally completed WHO breastfeeding assessment forms. Breastfeeding counselling was provided using a ‘45 points of counselling’ card developed over several years of learning in this programme (Box 1). Target weight gain was minimum 30g/day for babies under three months of age and 20g/day for babies between four and six months old. If target weight gain was not achieved, further breastfeeding counselling was provided, with follow-up after 48 hours, either in-clinic or at home. Once the mother was comfortable and target weight achieved for two consecutive visits 48 hours apart, the child was referred for monthly follow-up. During clinic visits mothers and infants were provided with vitamin supplements and mothers were counselled on newborn safety, exposure to the sun to raise vitamin D levels, developmental activities, home remedies for illness and protocols for antibiotic use (to prevent over-the-counter use of antibiotics for viral illness). A prophylactic dose of iron was given to infants from four months of age to prevent anaemia. Very few non-breastfed infants were seen in the clinic; where this happens, support is given for relactation.
Complementary feeding support: Mothers of babies over six months of age were given one-on-one counselling on complementary feeding using information, education and communication charts designed for caregivers and pregnant and lactating mothers. Strict follow-up was carried out every two weeks from six to eight months of age. Once mothers were following minimum adequate dietary advice and the baby was showing healthy growth, children were referred for monthly follow-up until reaching three years of age. Iron and vitamin supplements were given to this age group. During the initial years of the programme, it was noted that the growth of infants of complementary feeding age (over six months of age) often plateaued; this was seen most often in children of vegetarian households. To sustain weight and length gain and prevent growth faltering, vegetarian mothers were counselled to prepare nutrient-dense powders at home using peanut, sesame or other seeds, germinated or roasted beans and amylase to add to foods for their infants. Non-vegetarian mothers were counselled to include eggs, fish, chicken, liver and red meat to their infant’s diet from six months onwards. Following the introduction of this counselling, we observed that children over six months old continued to grow well and those with growth faltering quickly recovered. Counselling was supported with age-appropriate recipe booklets in local languages for mothers of infants at six, eight and 12 months of age.
Weekly cooking demonstrations were carried out with mothers of infants of complementary feeding age, as well as pregnant mothers. Recipes using locally available, cheap, nutrient-dense foods were used and cooked meals were fed to the children. During sessions, responsive feeding, consistency, dietary diversity and hygiene practices were discussed. Anaemia was checked at one year of age using portable HemoCue machines (for point-of-care haematology testing) and children were treated with a therapeutic dose of iron if they were found to be anaemic. From one year of age, children were given deworming medicines twice per year.
Counselling and support for pregnant mothers: Pregnant mothers attended the clinic regularly for weight monitoring and one-to-one counselling on nutritious diets. A weekly supply of clinic-made nutrient bars was provided, as well as iron and calcium supplements. Women were encouraged to join pregnancy clubs for group discussions on various topics related to pregnancy, including nutrition, breastfeeding and newborn-care training. Once the infant was born, field officers visited registered mothers in hospitals to guide them in early initiation of breastfeeding, positioning and attachment. On discharge, breastfeeding support was provided through regular home and clinic visits.
Home visits: Home visits were an integral part of the programme and involved visits by FMCH team members for one-on-one counselling of pregnant women and caregivers on maternal, infant and young child feeding hygiene, and to help families access more support if needed. Mother and infant pairs were also encouraged to attend ‘Mummy and Me’ classes on infant and child development, including communication, massage and play.
Development of tools: Recently, FMCH has started using advanced information, communication and technology tools, such as the Health Spoken Tutorials prepared by the Spoken Tutorial Project of the India Institute of Technology (IIT) and guided by the experience of FMCH programme staff. The Health Spoken Tutorial educational content portal1 and its YouTube channel offer self-paced, multilingual tutorials for pregnant women and caregivers on breastfeeding skills, complementary feeding, maternal nutrition, adolescent nutrition and infant care topics. Women who have access to smart phones watch the content at home or in the clinic. The videos were well received by women in FMCH clinics, with positive feedback on their success in supporting good breastfeeding technique.
Monitoring and lesson learning
Protocols were supported by customised, cloud-based software programs that included all relevant forms, including those for WHO breastfeeding assessment, well child, diet, severe acute malnutrition/moderate acute malnutrition management, home visits and activities. Software also supported the calculation of WHO z-scores and percentile growth charts. This enabled the efficient collation of data for individual and programme-monitoring purposes. Since the customised software was cloud-based, data could be remotely monitored in real-time by the team, including the clinic doctor, to ensure that each child was followed up appropriately and growth faltering identified and addressed. Challenging cases were immediately referred to the team doctor and nutritionist for appropriate, urgent action.
Monitoring data revealed many common problems experienced by mothers, such as poor breastfeeding positioning and attachment, and infrequent feeding. This detailed information helped the team tailor the ‘45 points of counselling’ card to address the most common issues faced and enable effective decision making.
Box 1. 45 counselling points for effective breastfeeding
Mother’s preparation
• Wash hands with soap and water and dry hands
• Drink boiled and cooled water
• Sit on the floor or bed or chair with proper back support
• Keep back straight
• Keep shoulders relaxed (not elevated/curved)
• Uncover the breast
• No pressure of bra/blouse on the breast
• Unwrap the baby from a blanket while feeding
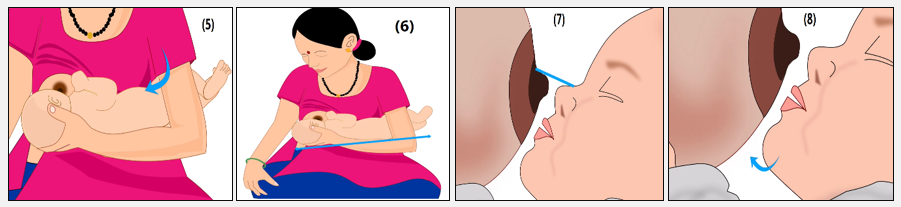
• Hold the baby’s head by the hand opposite the breast used to feed the baby (Image 1)
• Tuck baby’s legs under armpit of opposite hand (Image 2)
• Elevate baby to reach the breast (Image 3)
Position of mother’s thumb and fingers
• Mother’s thumb behind one ear and rest of the fingers behind the other ear of the baby; fingers should not be on the neck or pushing the head
• Wrist should rest between baby’s shoulder blades (Image 4)
Baby’s position
• Body should be gently pressed against the mother’s body (Image 5)
• Head, neck and body should be in a straight line (Image 6)
• Nose should be in the line with the nipple (Image 7)
• Baby’s full body should be supported
• Chin should be brought forward and close to the breast by extending the neck out a little (Image 8)
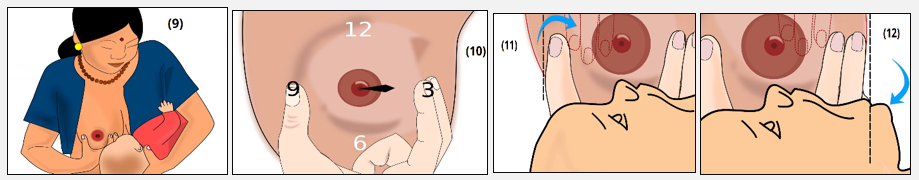
Holding breast while helping baby to latch the baby• Cup the breast underneath with a U-shaped hold (using the hand on the same side of the breast that the baby is feeding from) (Image 9)
• Mother’s one finger should be at the 9:00 o’clock position on the breast and other finger should be at the 3:00 o’clock position (Image 10)
• Thumb and fingers should be at a three-finger distance from the nipple (Images 11 & 12)
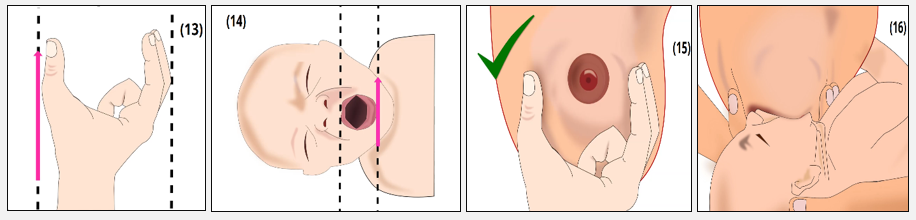
• Mother’s fingers should be parallel to the baby’s lips (Images 13 & 14)• Compress the breast while latching the baby so that the areola can be contoured and baby can get a large part of lower areola in the mouth (Images 15 &16)
• Equal compression of breast using thumb and fingers
• Avoid V-shaped compression, which will result in nipple feeding
Latching
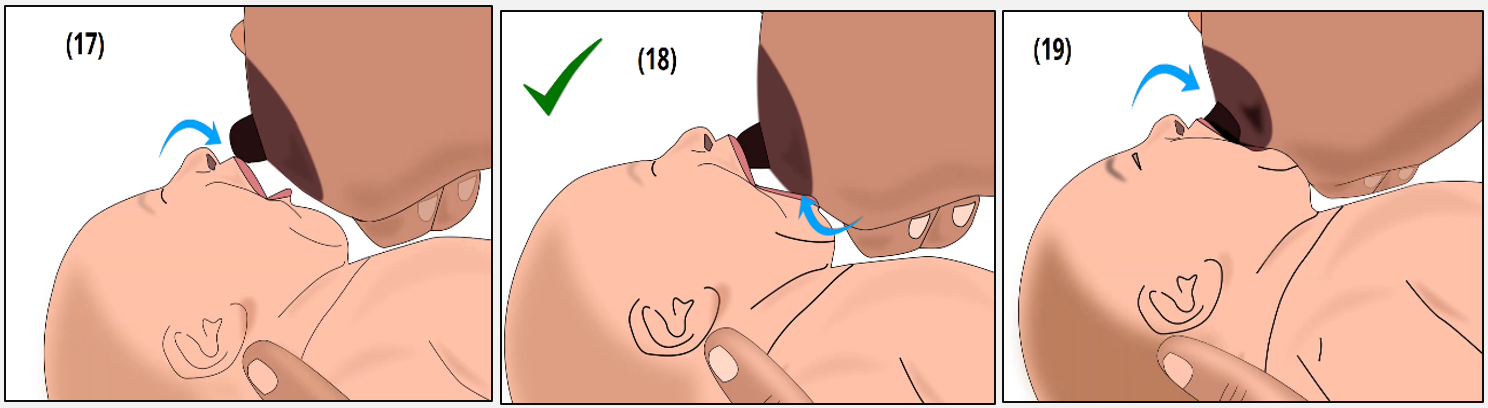
• To open the baby’s mouth wide, mother should touch her nipple to baby’s upper lip (Image 17)
• When baby opens her/his mouth wide, glide the breast into the mouth (sometimes this may take a few minutes, but it is of utmost importance to wait patiently for the baby to open her/his mouth wide
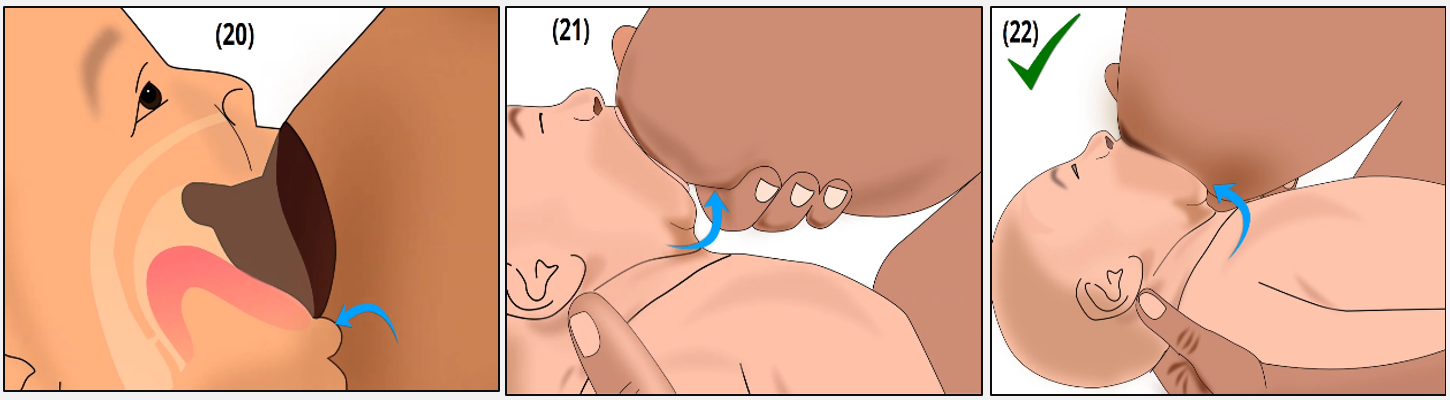
• Two-point latch. Latch the lower lip first, then the upper lip. The upper lip should be resting just above the nipple and the lower lip should be resting at the border of the areola and the breast (Images 18 & 19)
• Lower lip curved outwards (Image 20)
• In big breasts/well attached baby, press breast upward near the lower lip to check if significant part of lower areola is in the mouth (Image 21)
• Chin should be embedded well in the breast (Image 22)
Other counselling points
• Feed from one breast completely before offering the other
• To see if the first breast is completely emptied, express a little milk and check it. If the milk is watery and thin, or if thick milk is flowing copiously, continue to feed from the same side
• Give both foremilk (thin, watery milk made up of protein) and hind milk (thick, yellowish made up of fats) to the baby
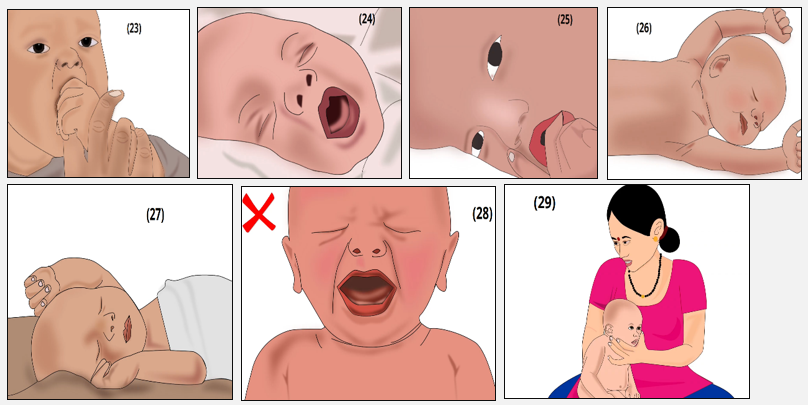
• Burp baby before offering the other breast. The best position to burp the baby is in sitting position, where the baby’s jaw is supported by the mother’s fingers and the baby’s chest is supported by the mother’s palm (Image 29)
• Wake up the baby if he/she falls asleep while feeding by tickling the feet, back, behind the ears, or making baby sit in burping position
• Use clean little finger to release the baby’s hold on the breast in case the baby latches onto the nipple or falls asleep on the breast
• If baby’s nose is pressed on the breast, extend the head slightly. Do not pull the baby off the breast
• Signs of proper latching: baby’s cheeks are filled and do not dimple, no fast suckling sound, jaw drops slowly and distinctly
• Breastfeed 8-12 times in 24 hours as per hunger cues in the first two to three months, then the frequency decreases
• Breastfeed two to three times at night
• Feed the baby on early hunger cues (these are squirming, stretching or opening the mouth); if the baby cries, it is too late (Images 23-28)
• Growth periods (when the baby’s demand for feeding will increase) occur at two weeks, six weeks and three months. Feed frequently during periods of increased demand
• Continue exclusive breastfeeding to six months of age, then continue breastfeeding with nutrient-dense complementary foods to at least two years of age or longe
Programme impact
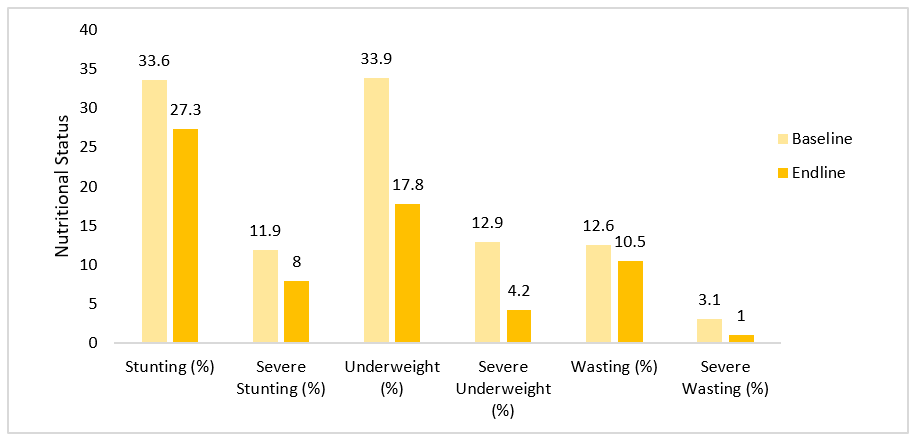
An analysis of baseline and endline malnutrition indicators was undertaken between 2013-2016 for all children who entered the programme under six months of age until at least their first birthday (286 children:153 boys and 133 girls). These children were selected based on age at registration (< 6 months), breastfeeding status (exclusively breastfed) and availability of follow-up data between 12 and 24 months of age. Length-for-age (LAZ), weight-for-age (WAZ) and weight-for-length (WHZ) z-scores were recorded at 0-6 months (baseline) and at 12-24 months of age (endline) for each child and prevalence levels of undernutrition calculated (Figure 5). Average age was 2.2 months at baseline and 13.9 months at endline.
In this cohort the prevalence of wasting, underweight and stunting were reduced between the baseline and endline periods. The decreases were particularly high for prevalence of underweight (decline by 47.5% in WAZ) compared to stunting (decline by 18.7% in LAZ) and wasting (decline by 16.7% in WHZ). Severe wasting declined by 67.7%, severe underweight by 67.4% and severe stunting by 32.7%. The progress in reduction in undernutrition over this short period (1 to 1.5 years) was high for stunting (6.3 percentage points) and underweight (16.1 percentage points). As there was no control group (this was not set up a research study), data from NFHS-4 (2016/17)2 helped contextualise the findings. Cautious comparison suggests a considerably lower prevalence of undernutrition amongst the intervention group compared to prevalence amongst a similar age group (13-24 months), the lowest quintile of the urban sample at state level (27.3% v 42.6% stunting, 17.8% v 35.4% underweight and 10.5% v 26.5% wasting at 13-24 months of age).
Figure 5: Baseline and endline nutrition status of a sub-sample of children (n=286) registered with FMCH at Ganesh Nagar, Ramdev Nagar and Sukhawani
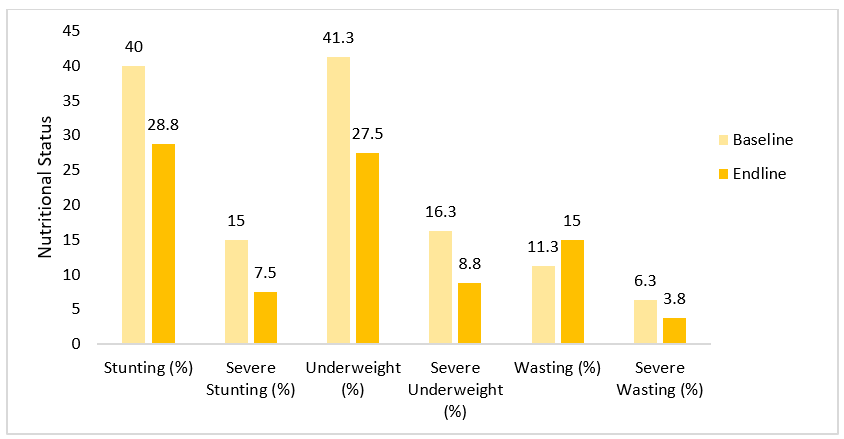
Data was collected from a sub-sample of 80 children of the same cohort for whom data was available from 24 months of age onwards to understand the longer-term impact of the programme on its beneficiaries. Data was analysed to compare prevalence of stunting, underweight and wasting between baseline (0-6 months) and endline (>24-35 months). The average age at endline of this sample was 25.9 months. In this population a reduction of 28.1% was seen in prevalence of stunting, 50% in severe stunting, 33.3% in underweight, 46.2% in severe underweight and 40% in severe wasting (Figure 6). However, there was an increase of 33.3% in wasting. Similarly, prevalence of undernutrition in this older sub-sample was considerably lower compared to children of similar age (25-36 months) in the poorest quintile for the urban state sample (28.8% v 39.9% stunting, 27.5% v 42.2% underweight, 15% v 23.6% wasting) (NFHS4, 2016/17).
Figure 6: Baseline and endline nutrition status of a sub-sample of children (n=80) registered with FMCH at Ganesh Nagar, Ramdev Nagar and Sukhawani over three years
Case study 1
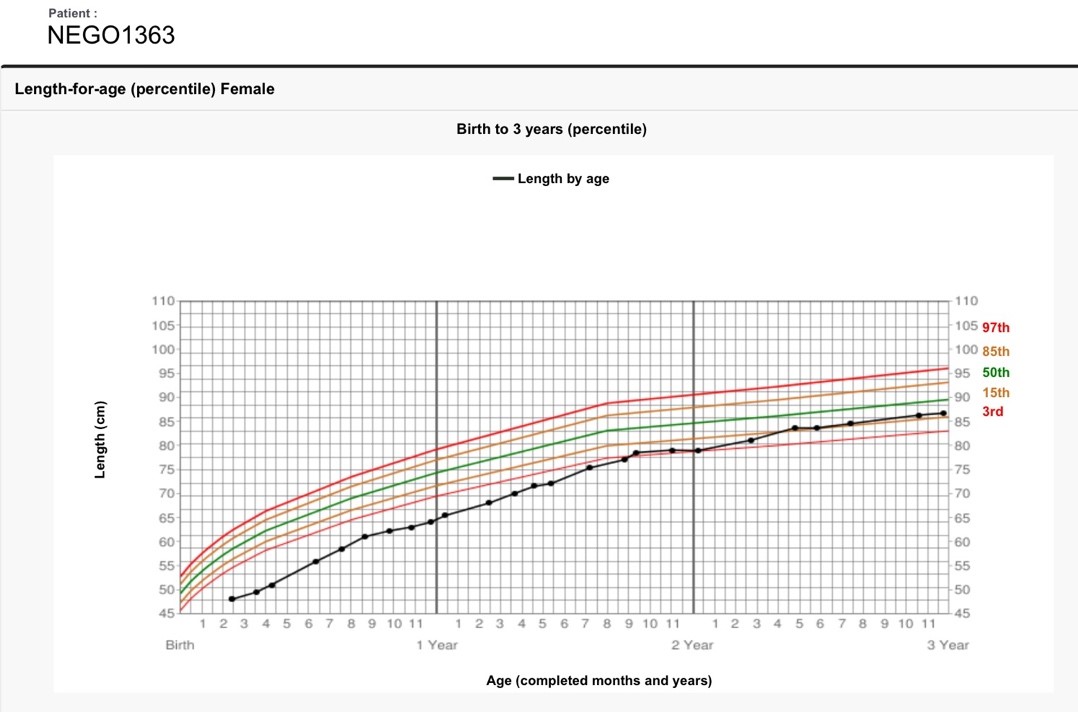
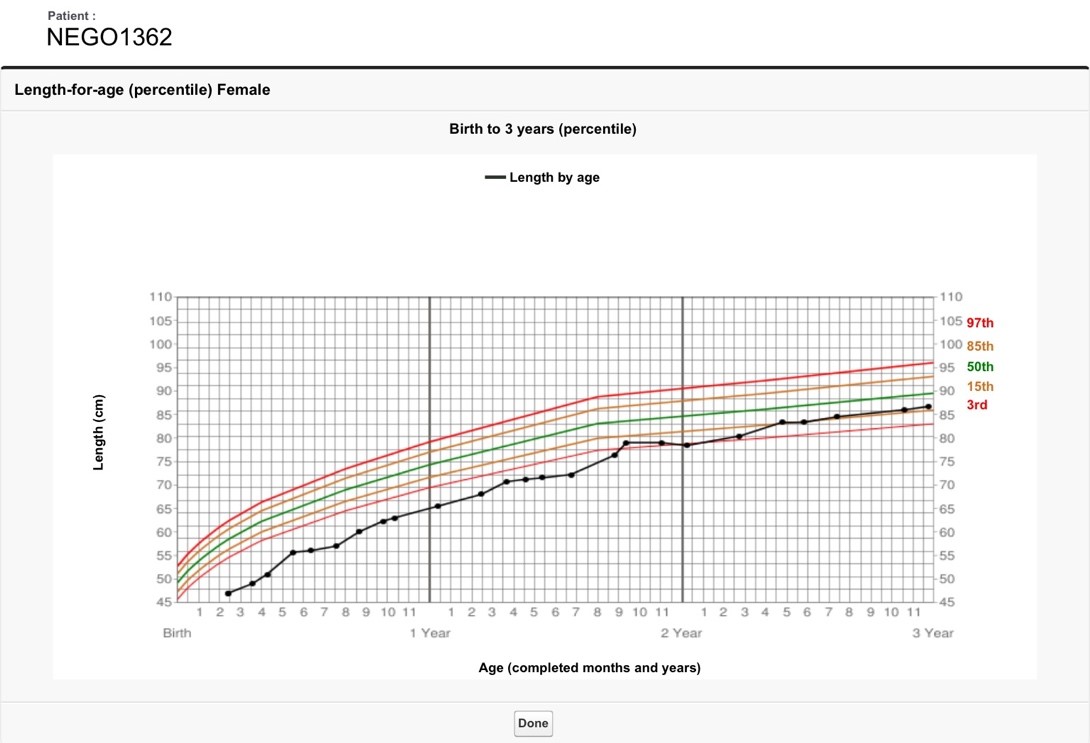
The first two growth charts below are of twin girls who were admitted to the clinic at around two months of age. They were severely stunted at the time of admission (height-for-age Z-scores (HAZ) nearly <-6 SD), as reflected in their World Health Organization (WHO) percentile growth chart. Their mother received counselling in breastfeeding and complementary feeding from six months of age. Response was much slower than experienced with other children; however, over time, both girls gained slow and steady length and their stunting was reversed by the time they were 27 months of age.
18-month-old twin girls who were admitted to the programme at two months of age and who had reversal of stunting by 27 months of age
Case study 2
An infant baby girl was admitted at two weeks of age. She was underweight and severely stunted at time of admission. The mother received counselling on breastfeeding and complementary feeding from six months of age. The child’s WHO weight-for-age (WFA) percentile chart demonstrates that her weight reached 50th percentile at around seven months of age and she had constant linear growth recovery, as seen in the second chart below, a length-for-age percentile chart, until two years of age.
Building the capacity of the government health workforce
Maternal and infant and young child feeding training was recently provided to government health workers in the Department of Health and Department of Women and Child Development in tribal areas of Melghat, Maharashtra. Online Health Spoken Tutorials were used to train medical officers, Anganwadi supervisors, counsellors and block facilitators on a range of topics (Box 2). Trainees were equipped to cascade this training to other government health workers who provide counselling to mothers. After completion of training, participants took a written exam, attended a practical workshop with demonstrations using a model breast and doll, and received practical training from a supervisor. Participants were tasked with following 10 babies for one month (with remote support via WhatsApp and referral of non-responsive cases to the medical officer). The cost of the training was minimal as it used free online tutorials, with practical sessions using low-cost tools.
Data from infants monitored and counselled by newly trained government health workers from the Department of Health in Banaskantha district in Gujarat (medical officers, auxiliary nurse midwives and accredited social health activists) demonstrate early success of the training programme, with many infants reported to be gaining over 40g per day. Figure 7 presents data of 51 infants who received counselling from newly trained health workers from Banaskantha district with at least four weekly follow-ups who were between 26-31 days of age at their last visit. This shows that, between birth and last follow-up, over 62% of infants gained 30g or more weight per day and almost 8% gained 60g or more per day, with mean weight gain of 37g/day.
Another cohort was analysed of infants (n=154) who entered their fourth week of life (aged >21 days) for whom data was available. Of these infants, 17.5% (n=27) were born with a weight of < 2.5kg (LBW). Among the 40 infants with a record from their first week of life, mean weight gain was negative at -7.7g/day; mean weight gain for infants with a record in their second week (n=106) was 22.3 g/day; in their third week (n=101) 40.5g/day; and in their fourth week (n=107) 42.6g/day (Figure 8). Results highlight the importance of effective breastfeeding training.
Box 2: Training topics covered in government health worker training
- Breastfeeding skills and the science behind it (3 hours)
- Type 1 & Type 2 nutrients and the first 1,000 Days (2 hours)
- Pre-pregnancy and maternal nutrition to decrease low birth weight and pregnancy charts (1 hour)
- Complementary foods (2 hours)
- Growth charts/child growth tracker (2 hours)
- Breast crawl and kangaroo mother care (2 hours)
- Expressing, storing and feeding expressed breastmilk (2 hours)
- Nipple and breastfeeding problems and physical methods to increase milk supply (2 hours)
- Practical workshop
Figure 7: Infant progress according to weight gain from birth to last follow-up between 26-31 days (%) (n=51)
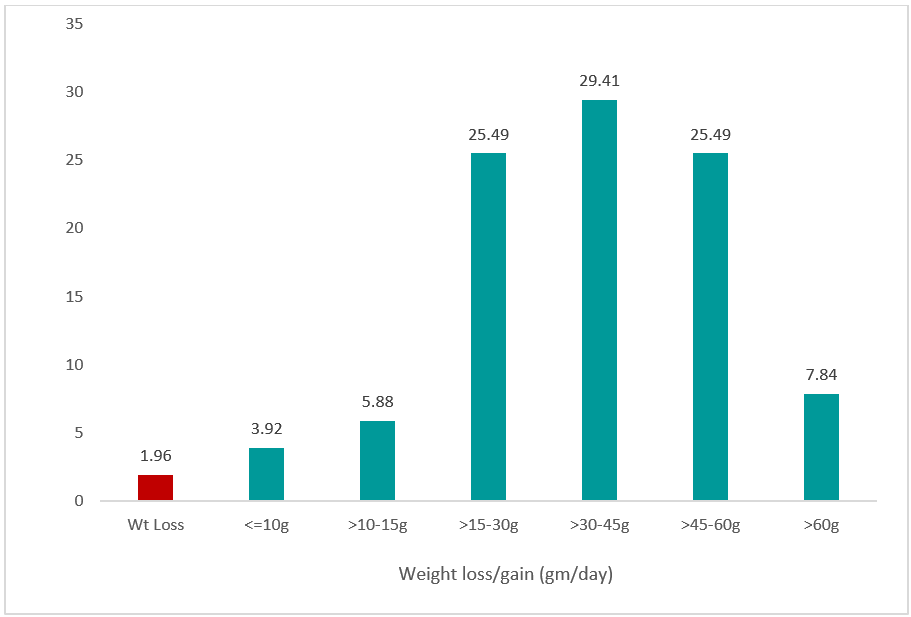
Figure 8: Mean weight gain (g/day) by week for a cohort of infants >21 days old (n=154)
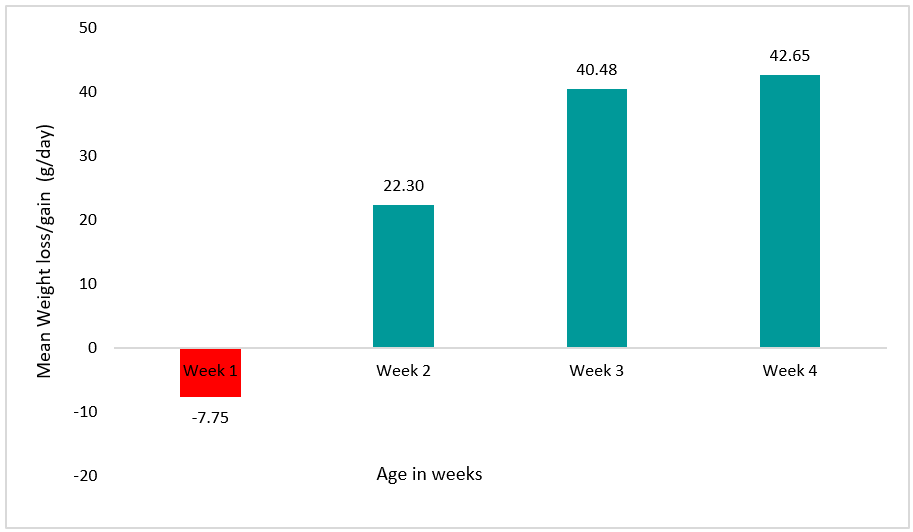
Note*: If multiple visits in a given week, the first visit data was considered
Discussion
Contextualised, targeted, quality counselling focusing on critical moments in the lifecycle is necessary and effective. The Foundation for Mother and Child Health programme developed a set of protocols and accompanying tools tailored to needs and challenges faced by caregivers in this context. This included online videos created by the India Institute of Technology (IIT) Bombay to support counselling targeted to key points in the lifecycle (pregnancy, infants under six months exclusively breastfeeding, and infants and young children of complementary feeding age). The ‘cross-cradle hold’ and ‘45 points of counselling card’ were critical to the success of this intervention. The experience highlights the importance of a deep understanding of the issues faced in a specific context and the development of protocols and tools that respond to these. The experience also demonstrates the importance of empowering pregnant and lactating women and caregivers with information so that they understand why and how actions should be taken to achieve optimal growth of their infants.
Accurate weight monitoring is critical to track progress and inform early action. The programme highlights the need for frequent, accurate weight monitoring to identify and address growth faltering early on, before an infant becomes wasted. In this programme, weight monitoring was successfully supported by the use of cloud-based software (in this case, Veracross) that plotted babies’ growth on the World Health Organization growth chart and calculated their z-scores and percentile growth. This provided time efficiencies, avoided human error, and enabled the immediate, remote identification of growth faltering to support quick action. Active weight monitoring in early infancy was also supported by frequent home visits.
Technology can help support programming and monitoring. Technology was used to support one-to-one counselling and breastfeeding assessments and to collate data on complementary feeding, as well as for weight monitoring. This enabled understanding of common issues and trends and the adaptation of protocols in response. The use of online videos for mothers and the training of health workers also proved an extremely effective way of providing low-cost support to large numbers of individuals in a short space of time.
Training and supervision of the health workforce to support service quality is essential. Quality training and supervision of the health workforce, with referral mechanisms in place when children fail to respond, has been critical to the success of the FMCH programme, enabling consistency of messaging to mothers. The experience of training government health workers has shown that, with the use of online resources, training does not need to be costly and is possible within the existing health system in India.
Next steps
There are encouraging signs that the FMCH programme has had a positive impact on the prevention of stunting and wasting among beneficiary children in a relatively short space of time through a combination of intensive weight monitoring and contextualised, targeted counselling of pregnant and lactating mothers and caregivers. The FMCH programme has been successfully replicated in rural settings in Shrirampur, Maharashtra since 2013, as well as in the outskirts of Mumbai since 2017 through government integrated child development services in Anganwadi centres. This shows that there is potential to integrate the FMCH protocol into routine health services using existing personnel through a method of low-cost training based on free, online training resources. This type of intervention could assist the Government of India in achieving its wasting and stunting targets. FMCH is keen for more organisations and governments across the world to use the curriculum and methodology developed by the Spoken Tutorial team at the Indian Institute of Technology, Bombay and share resources and experiences.
For more information please contact Rupal Dalal.
References
International Institute for Population Sciences (IIPS) (2016a) National Family Health Survey (NFHS-4) 2015-16: India. Ministry of Health and Family Welfare.
International Institute for Population Sciences (2016b) India 2015-16 DHS-VII. DHS Programme.
IIT Bombay (N.D.) Spoken Tutorials Health & Nutrition. Available at: https://spoken-tutorial.org/series_tutorial-search/?search_otherfoss=Health+and+Nutrition
URBAN HUNGaMA, the HUNGaMA Survey Report, 2014. Available at: www.naandi.org/wp-content/uploads/Urban-HUNGAMA-Final-Report-1.pdf
1 https://spoken-tutorial.org/series_tutorial-search/?search_otherfoss=Health+and+Nutrition
2 Data will have been gathered in 2014/15, coinciding with the intervention programme data collection; hence this data was selected for contextualisation.